Abstract
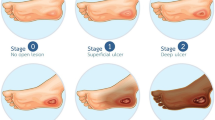
A 3D convolution neural network (CNN) of deep learning architecture is supplied with essential visual features to accurately classify and segment granulation, necrotic eschar, and slough tissues in pressure ulcer color images. After finding a region of interest (ROI), the features are extracted from both the original and convolved with a pre-selected Gaussian kernel 3D HSI images, combined with first-order models of current and prior visual appearance. The models approximate empirical marginal probability distributions of voxel-wise signals with linear combinations of discrete Gaussians (LCDG). The framework was trained and tested on 193 color pressure ulcer images. The classification accuracy and robustness were evaluated using the Dice similarity coefficient (DSC), the percentage area distance (PAD), and the area under the ROC curve (AUC). The obtained preliminary DSC of 92%, PAD of 13%, and AUC of 95% are promising.

The Classification of Pressure Ulcer Tissues Based on 3D Convolutional Neural Network.










Similar content being viewed by others
References
Mukherjee R, Manohar DD, Das DK, Achar A, Mitra A, Chakraborty C (2014) Automated tissue classification framework for reproducible chronic wound assessment. Biomed Res Int 2014:1–9
Fauzi MFA, Khansa I, Catignani K, Gordillo G, Sen CK, Gurcan MN (2015) Computerized segmentation and measurement of chronic wound images. Comput Biol Med 60:74–85. [Online]. Available: http://www.sciencedirect.com/science/article/pii/S0010482515000645
Sen CK, Gordillo GM, Roy S, Kirsner R, Lambert L, Hunt TK, Gottrup F, Gurtner GC, Longaker MT (2009) Human skin wounds: a major and snowballing threat to public health and the economy. Wound Repair Regen 17(6):763–771. [Online]. Available: https://doi.org/10.1111/j.1524-475X.2009.00543.x
Cuddigan J, Berlowitz DR, Ayello EA (2001) Pressure ulcers in america: prevalence, incidence, and implications for the future. Adv Skin Wound Care 14(4):208–215
Deprez JF, Cloutier G, Schmitt C, Gehin C, Dittmar A, Basset O, Brusseau E (2007) 3d ultrasound elastography for early detection of lesions. evaluation on a pressure ulcer mimicking phantom. In: 2007 29th annual international conference of the ieee engineering in medicine and biology society , pp 79–82
Agostini JV, Baker DI, Bogardus ST Making health care safer: A critical analysis of patient safety practices. Agency for Healthcare Research and Quality, U.S. Department of Health and Human Services, 2001, no. 27, ch. Prevention of Pressure Ulcers in Older Patients, pp 301–306
Leachtenauer J, Kell S, Turner B, Newcomer C, Lyder C, Alwan M (2006) A non-contact imaging-based approach to detecting stage i pressure ulcers. In: the proceedings of the 2006 international conference of the IEEE engineering in medicine and biology society, pp 6380–6383
Prado A, Andrades P, Benítez S Cirugía Plástica Esencial. Hospital Clinico Universidad De Chile, 2005, ch. Úlceras por presión, pp 111–126
Guadagnin R, Neves RD, Santana LA, Guilhem DB (2014) An image mining based approach to detect pressure ulcer stage. Pattern Recognit Image Anal 24(2):292–296. [Online]. Available: https://doi.org/10.1134/S1054661814020084
Beal ME, Smith K (2016) Inpatient pressure ulcer prevalence in an acute care hospital using evidence-based practice. Worldviews Evid-Based Nurs 13(2):112–117. [Online]. Available: https://doi.org/10.1111/wvn.12145
Dorileo AG, Frade MAC, Rangayyan RM, Azevedo-Marques PM (2010) Segmentation and analysis of the tissue composition of dermatological ulcers. In: CCECE 2010, pp 1–4
Veredas F, Mesa H, Morente L (2010) Binary tissue classification on wound images with neural networks and bayesian classifiers. IEEE Trans Med Imaging 29(2):410–427
Azevedo-Marques PM, Pereira SM, Frade MAC, Rangayyan RM (2013) Segmentation of dermatological ulcers using clustering of color components. In: 2013 26th IEEE Canadian conference on electrical and computer engineering (CCECE) , pp 1–4
Veredas FJ, Luque-Baena RM, Martín-Santos FJ, Morilla-Herrera JC, Morente L (2015) Wound image evaluation with machine learning. Neurocomputing 164:112–122
Ortiz DP, Sierra-Sosa D, Zapirain BG (2017) Pressure ulcer image segmentation technique through synthetic frequencies generation and contrast variation using toroidal geometry. BioMedical Engineering OnLine 16:1–19
Wang C, Yan X, Smith M, Kochhar K, Rubin M, Warren SM, Wrobel J, Lee H (2015 ) A unified framework for automatic wound segmentation and analysis with deep convolutional neural networks. In: 2015 37th annual international conference of the ieee engineering in medicine and biology society (EMBC), pp 2415–2418
Kawahara J, Hamarneh G (2016) Multi-resolution-Tract CNN with hybrid pretrained and skin-lesion trained layers. Springer International Publishing, Cham, pp 164–171
Esteva A, Kuprel B, Novoa RA, Ko J, Swetter SM, Blau HM, Thrun S (2017) Dermatologist-level classification of skin cancer with deep neural networks. Nature 542(7639):115–118. [Online]. Available: https://doi.org/10.1038/nature21056
Soliman A, Khalifa F, Elnakib A, El-Ghar MA, Dunlap N, Wang B, Gimel’farb G, Keynton R, El-Baz A (2017) Accurate lungs segmentation on CT chest images by adaptive appearance-guided shape modeling. IEEE Trans Med Imaging 36(1):263– 276
Lindeberg T (2011) Generalized Gaussian scale-space axiomatics comprising linear scale-space, affine scale-space and spatio-temporal scale-space. J Math Imaging Vis 40(1):36–81. [Online]. Available: https://doi.org/10.1007/s10851-010-0242-2
Kamnitsas K, Ledig C, Newcombe VF, Simpson JP, Kane AD, Menon DK, Rueckert D, Glocker B (2017) Efficient multi-scale 3d {CNN} with fully connected {CRF} for accurate brain lesion segmentation. Med Image Anal 36:61–78
El-Baz A, Elnakib A, Khalifa F, El-Ghar MA, McClure P, Soliman A, Gimelrfarb G (2012) Precise segmentation of 3-d magnetic resonance angiography. IEEE Trans Biomed Eng 59(7):2019–2029
Webb AR, Copsey KD (2011) Statistical pattern recognition, 3rd edn. Wiley, Hoboken
Thomas S (2017) Medetec wound database, http://www.medetec.co.uk/files/medetec-image-databases.html
Dice LR (1945) Measures of the amount of ecologic association between species. Ecology 26(3):297–302. [Online]. Available: http://www.jstor.org/stable/1932409
Powers DMW (2011) Evaluation: from precision, recall and f-measure to roc, informedness, markedness & correlation. J Mach Learn Technol 2(1):37–63
Yang Y, Huang S (2007) Image segmentation by fuzzy c-means clustering algorithm with a novel penalty term. Computing and informatics 26:17–31
Otsu N (1979) A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern 9 (1):62–66
Bland J, Altman D (1986) Statistical methods for assessing agreement between two methods of clinical measurement. Lancet 8:307–310
Acknowledgements
The authors thank Prof. Dr. Georgy Gimel’farb, Department of Computer Science, University of Auckland, Auckland, New Zealand, for his help in revising the paper. In addition, the authors want to thank Sofia Zahia, Connor Burns, and Daniel Sierra-Sosa for their support in summarizing the related work and preparing the masks for the GT images.
Funding
The grants that have contributed with partial funding of the study are IT − 905 − 16 to eVIDA research group from the Basque Government, JC2015 − 00305 Josè Castillejo Research Stay Grant from the Spanish Ministry, and ACM2017_09 from the University of Deusto.
Author information
Authors and Affiliations
Corresponding author
Additional information
The first and second authors contributed equally to this work and shared the first authorship.
The third and fourth authors are sharing the senior authorship.
Rights and permissions
About this article
Cite this article
García-Zapirain, B., Elmogy, M., El-Baz, A. et al. Classification of pressure ulcer tissues with 3D convolutional neural network. Med Biol Eng Comput 56, 2245–2258 (2018). https://doi.org/10.1007/s11517-018-1835-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-018-1835-y