Abstract
The hemodynamics conditioned by coronary geometry may play an important role in the creation of a pro-atherogenic environment in specific locations of the coronary tree. The aim of this study is to identify how several geometric parameters of the left coronary artery – cross-section areas, proximal left anterior descending artery length, angles between the branches and the septum, curvature and tortuosity – can be related with hemodynamic descriptors, using a computational fluid–structure interaction method. It is widely accepted that the hemodynamic indicators play an important role in identifying possible pro-atherogenic locations. A statistical study, using Pearson correlation coefficient and P value, was performed for a population study of 8 normal human left coronary arteries presenting right-dominant circulation. Within the study cases, arteries with high caliber (r = 0.88), high angles LMS-LAD (r = 0.49), LAD-LCx (r = 0.57) and LAD-Septum (r = 0.52), and high tortuosity LMS-LCx (r = 0.63) were correlated with a hemodynamic behavior propitious to plaque formation in the left anterior descending artery. In contrast, high proximal left anterior descending artery length (r = −0.41), high angle LMS-LCx (r = −0.59), high tortuosity LMS-LAD (r = −0.56) and LAD-LCx (r = −0.55) and high curvature of LMS (r = −0.60) and LCx (r = −0.56) can lead to non-favorable hemodynamic conditions for atheroma formation.

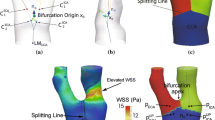
Graphical abstract












Similar content being viewed by others
Abbreviations
- CFD:
-
Computational fluid dynamics
- CT:
-
Computerized tomography
- FSI:
-
Fluid–structure interaction
- LAD:
-
Left anterior descending artery
- LCx:
-
Left circumflex artery
- LMS:
-
Left main stem
- LNH:
-
Localized normalized helicity
- OSI:
-
Oscillatory shear index
- RRT:
-
Relative residence time
- TAWSS:
-
Time-averaged wall shear stress
- WSS:
-
Wall shear stress
- A :
-
Pressure gradient
- A subscript (mm2):
-
Cross-section area of the subscript
- a 10, a 01, a 20, a 11, a 02 (MPa):
-
Hyperelastic constants
- D (m):
-
Diameter of the artery
- d (MPa−1):
-
Incompressible parameter
- d i − j (mm):
-
Centerline distance between i and j
- d w (mm):
-
Distance from the wall
- h (mm):
-
Slice thickness
- I 1, I 2 :
-
First and second strain invariants
- J :
-
Elastic volume ratio
- J 0 :
-
First-order Bessel Function
- L i − j (mm):
-
Shortest distance between i and j
- l subscript (mm):
-
Length of the subscript
- max i :
-
Maximum of i
- \( {\dot{m}}_i \) (kg.s):
-
Mass flow rate through i
- n c :
-
Sample size
- n :
-
Flow constant, Carreau model
- P(t) (mmHg):
-
Imposed pressure profile
- p(t) (mmHg):
-
Pressure profile
- p diastole (mmHg):
-
Diastolic pressure
- R (mm):
-
Artery radius
- r :
-
Pearson correlation coefficient
- r d (mm):
-
Radial distance from the artery axis to a given point
- Re :
-
Reynolds number
- s :
-
Artery wall location
- s arc (mm):
-
Arc length
- \( \overrightarrow{T} \) :
-
Unit target length
- T (s):
-
Time of the total cardiac cycle
- t (s):
-
Time instance
- V(x, t):
-
Velocity vector
- V m (m/s):
-
Mean velocity
- \( {V}_{in}^m \) (cm/s):
-
Mean inlet velocity profile
- W (J/m3):
-
Strain energy–density function
- # i :
-
Number of i
- α :
-
Womersley number
- α i − j (°):
-
Angle between i and j
- \( \dot{\gamma} \) (s−1):
-
Shear rate
- κ i − j (mm−1):
-
Curvature between i and j
- λ (s):
-
Relaxation time
- μ :
-
Mean value
- μ f (Pa.s):
-
Blood dynamic viscosity
- μ OSI :
-
Mean OSI value
- μ RRT [Pa−1]:
-
Mean RRT value
- μ TAWSS [Pa]:
-
Mean TAWSS value
- μ 0 (Pa.s):
-
Zero shear viscosity
- μ ∞ (Pa.s):
-
Infinite shear viscosity
- ρ (kg/m3):
-
Density
- ρ f (kg/m3):
-
Blood density
- ρ w (kg/m3):
-
Arterial wall density
- σ :
-
Standard deviation
- τ i − j (%):
-
Tortuosity between i and j
- ω (rad.s−1):
-
Cardiac pulse frequency
- ω(x, t) (s−1):
-
Vorticity vector
References
(2010) WHO | The Atlas of Heart Disease and Stroke. WHO
Bentzon JF, Otsuka F, Virmani R, Falk E (2014) Mechanisms of plaque formation and rupture. Circ Res 114:1852–1866. https://doi.org/10.1161/CIRCRESAHA.114.302721
Wilson PWF, D’Agostino RB, Levy D et al (1998) Prediction of coronary heart disease using risk factor categories. Circulation 97:1837–1847. https://doi.org/10.1161/01.CIR.97.18.1837
Malvè M, Gharib AM, Yazdani SK et al (2014) Tortuosity of coronary bifurcation as a potential local risk factor for atherosclerosis: CFD steady state study based on in vivo dynamic CT measurements. Ann Biomed Eng 43:82–93. https://doi.org/10.1007/s10439-014-1056-y
Caro CG, Fitz-Gerald JM, Schroter RC (1969) Arterial wall shear and distribution of early atheroma in man. Nature 223:1159–1161. https://doi.org/10.1038/2231159a0
Karimi A, Navidbakhsh M, Shojaei A et al (2014) Study of plaque vulnerability in coronary artery using Mooney–Rivlin model: a combination of finite element and experimental method. Biomed Eng Appl Basis Commun 26:1450013. https://doi.org/10.4015/S1016237214500136
Karimi A, Navidbakhsh M, Faghihi S et al (2012) A finite element investigation on plaque vulnerability in realistic healthy and atherosclerotic human coronary arteries. Proc Inst Mech Eng H 227:148–161. https://doi.org/10.1177/0954411912461239
Chaichana T, Sun Z, Jewkes J (2012) Computational fluid dynamics analysis of the effect of plaques in the left coronary artery. Comput Math Methods Med 2012. https://doi.org/10.1155/2012/504367
Chaichana T, Sun Z, Jewkes J (2011) Computation of hemodynamics in the left coronary artery with variable angulations. J Biomech 44:1869–1878. https://doi.org/10.1016/j.jbiomech.2011.04.033
Pinto S, Campos JBLM (2016) Numerical study of wall shear stress-based descriptors in the human left coronary artery. Comput Methods Biomech Biomed Engin 19:1443–1455. https://doi.org/10.1080/10255842.2016.1149575
Costa ED (2016) Hemodynamics in the Left Coronary Artery – numerical and in vitro approaches. Retrieved from Repositório Aberto da Universidade do Porto
Doutel E, Pinto SIS, Campos JBLM, Miranda JM (2016) Link between deviations from Murray’s law and occurrence of low wall shear stress regions in the left coronary artery. J Theor Biol 402:89–99. https://doi.org/10.1016/j.jtbi.2016.04.038
Malvè M, García A, Ohayon J, Martínez MA (2012) Unsteady blood flow and mass transfer of a human left coronary artery bifurcation: FSI vs. CFD. Int Commun Heat Mass Transf 39:745–751. https://doi.org/10.1016/j.icheatmasstransfer.2012.04.009
Dong J, Sun Z, Inthavong K, Tu J (2015) Fluid–structure interaction analysis of the left coronary artery with variable angulation. Comput Methods Biomech Biomed Engin 18:1500–1508. https://doi.org/10.1080/10255842.2014.921682
Guerciotti B, Vergara C, Ippolito S et al (2017) A computational fluid–structure interaction analysis of coronary Y-grafts. Med Eng Phys 47:117–127. https://doi.org/10.1016/j.medengphy.2017.05.008
Zhu H, Friedman MH (2003) Relationship between the dynamic geometry and wall thickness of a human coronary artery. Arterioscler Thromb Vasc Biol 23:2260–2265. https://doi.org/10.1161/01.ATV.0000095976.40874.E0
Johnston BM, Johnston PR (2007) The relative effects of arterial curvature and lumen diameter on wall shear stress distributions in human right coronary arteries. Phys Med Biol 52:2531–2544. https://doi.org/10.1088/0031-9155/52/9/013
Zakaria H, Robertson AM, Kerber CW (2008) A parametric model for studies of flow in arterial bifurcations. Ann Biomed Eng 36:1515–1530. https://doi.org/10.1007/s10439-008-9531-y
Sousa LC, Castro CF, António CC et al (2014) Toward hemodynamic diagnosis of carotid artery stenosis based on ultrasound image data and computational modeling. Med Biol Eng Comput 52:971–983. https://doi.org/10.1007/s11517-014-1197-z
Womersley JR (1955) Method for the calculation of velocity, rate of flow and viscous drag in arteries when the pressure gradient is known. J Physiol 127:553–563. https://doi.org/10.1113/jphysiol.1955.sp005276
Park CG, Lee JY (2011) The significance of the J-curve in hypertension and coronary artery diseases. Korean Circ J 41:349–353. https://doi.org/10.4070/kcj.2011.41.7.349
Torii R, Wood NB, Hadjiloizou N et al (2009) Fluid–structure interaction analysis of a patient-specific right coronary artery with physiological velocity and pressure waveforms. Commun Numer Methods Eng 25:565–580. https://doi.org/10.1002/cnm.1231
Pinto SIS, Campos JBLM, Azevedo E et al (2018) Numerical study on the hemodynamics of patient-specific carotid bifurcation using a new mesh approach. Int J Numer Method Biomed Eng 34:e2972. https://doi.org/10.1002/cnm.2972
Zhang Q, Gao B, Chang Y (2016) Effect of different rotational directions of BJUT-II VAD on aortic swirling flow characteristics: a primary computational fluid dynamics study. Med Sci Monit 22:2576–2588. https://doi.org/10.12659/MSM.899313
Gao H, Long Q, Graves M et al (2009) Carotid arterial plaque stress analysis using fluid-structure interactive simulation based on in-vivo magnetic resonance images of four patients. J Biomech 42:1416–1423. https://doi.org/10.1016/j.jbiomech.2009.04.010
Ansys® Academic Research 15.0 (2013) ANSYS fluent tutorial guide. Help Syst:1067
Pinho N, Bento M, Sousa LC et al (2018) In: Natal Jorge RM, Tavares JMRS (eds) Patient-specific study of a Stenosed carotid artery bifurcation using fluid–structure interactive simulation BT - VipIMAGE 2017: proceedings of the VI ECCOMAS thematic conference on computational vision and medical image processing Porto, Portugal, Octob. Springer, Cham, pp 495–503
AM M, SL A, Izumo S (1999) Hemodynamic shear stress and its role in atherosclerosis. JAMA 282:2035–2042
Tarbell JM (2003) Mass transport in arteries and the localization of atherosclerosis. Annu Rev Biomed Eng 5:79–118. https://doi.org/10.1146/annurev.bioeng.5.040202.121529
Soulis J V, Fytanidis DK (2011) Oscillating shear index , wall shear stress and low density lipoprotein accumulation in human RCAs. 3rd Micro and Nano Flows Conference, Thessaloniki, Greece, 22–24 August 2011
He X, He X, Ku DN, Ku DN (1996) Pulsatile flow in the human left coronary artery bifurcation: average conditions. J Biomech Eng 118:74–82
Arzani A, Gambaruto AM, Chen G, Shadden SC (2017) Wall shear stress exposure time: a Lagrangian measure of near-wall stagnation and concentration in cardiovascular flows. Biomech Model Mechanobiol 16:787–803. https://doi.org/10.1007/s10237-016-0853-7
Gallo D, Isu G, Massai D et al (2014) A survey of quantitative descriptors of arterial flows BT - visualization and simulation of complex flows in biomedical engineering. In: Imai Y, Ishikawa T, Oliveira MSN (eds) Lima R. Springer, Dordrecht, pp 1–24
Lee S-W, Antiga L, Steinman DA (2009) Correlations among indicators of disturbed flow at the normal carotid bifurcation. J Biomech Eng 131:061013. https://doi.org/10.1115/1.3127252
Lorenz R, Bock J, Barker AJ et al (2014) 4D flow magnetic resonance imaging in bicuspid aortic valve disease demonstrates altered distribution of aortic blood flow helicity. Magn Reson Med 71:1542–1553. https://doi.org/10.1002/mrm.24802
Munson BR, Okiishi TH, Huebsch WW, Rothmayer AP (2013) Fundamentals of fluid mechanics. Wiley, Hoboken
Dahiru T (2011) P-value, a true test of statistical significance? A cautionary note. Ann Ibadan Postgrad Med 6:21–26. https://doi.org/10.4314/aipm.v6i1.64038
Evans JD (1995) Straightforward statistics for the behavioral science. Brooks/Cole, Pacific Grove
Wasilewski J, Niedziela J, Osadnik T et al (2015) Predominant location of coronary artery atherosclerosis in the left anterior descending artery. The impact of septal perforators and the myocardial bridging effect. Kardiochir Torakochirurgia Pol 12:379–385. https://doi.org/10.5114/kitp.2015.56795
Acknowledgments
The authors gratefully acknowledge the Foundation for Science and Technology Portugal (FCT), the Research Unit LAETA-INEGI, the Engineering Faculty of University of Porto, and the Cardiovascular R&D Unit of the Medicine Faculty of University of Porto.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pinho, N., Castro, C.F., António, C.C. et al. Correlation between geometric parameters of the left coronary artery and hemodynamic descriptors of atherosclerosis: FSI and statistical study. Med Biol Eng Comput 57, 715–729 (2019). https://doi.org/10.1007/s11517-018-1904-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-018-1904-2