Abstract
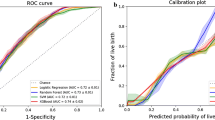
Infertility has become a global health problem, increasing the number of couples looking for in vitro fertilization (IVF). Despite advances and technical improvements, some couples remain childless due to the high complexity of the technique. The use of machine learning (ML) in the prediction of pregnancy, computing factors that could interfere in the effectiveness of the treatment, is an important tool to optimize these factors and reach the success of pregnancy. The aim of this study was to apply ML models to determine variables related to pregnancy after IVF in a public health service, including pre-implantation variables. This study included 771 women who underwent IVF treatment at Hospital das Clínicas, Federal University of Minas Gerais, between 2013 and 2019. We used the following Machine Learning algorithms: Logistic Regression, Random Forest, XG Boost and Support Vector Machines. The Random Forest algorithm achieved the best performance, with better accuracy, sensitivity and area under the ROC curve to predict the success of IVF evaluated by pregnancy frequency. We also trained a specific model only for women older than 35 years old.
Graphical abstract
Variables in the Random Forest model related to pregnancy after in vitro fertilization







Similar content being viewed by others
References
Zegers-Hochschild F et al (2009) The International Committee for Monitoring Assisted Reproductive Technology (ICMART) and the World Health Organization (WHO) revised glossary on ART terminology, 2009. Hum Reprod 24(11):2683–2687
Kumar N, Singh AK (2015) Trends of male factor infertility, an important cause of infertility: a review of literature. Journal of Human Reproductive Sciences 8(4):191
Kaufmann S, Eastaugh J, Snowden S, Smye S, Sharma V (1997) The application of neural networks in predicting the outcome of in-vitro fertilization. Human Reproduction (Oxford, England) 12(7):1454–1457
Ramasamy, N. et al. Feature reduction by improvised hybrid algorithm for predicting the IVF success rate. International Journal of Advanced Research in Computer Science 8 (1) (2017)
Hassan MR, Al-Insaif S, Hossain MI, Kamruzzaman J (2020) A machine learning approach for prediction of pregnancy outcome following IVF treatment. Neural Comput Appl 32(7):2283–2297
Hafiz P, Nematollahi M, Boostani R, Jahromi BN (2017) Predicting implantation outcome of in vitro fertilization and intracytoplasmic sperm injection using data mining techniques. International journal of fertility & sterility 11(3):184
Blank C et al (2019) Prediction of implantation after blastocyst transfer in in vitro fertilization: a machine-learning perspective. Fertil Steril 111(2):318–326
Khosravi P et al (2019) Deep learning enables robust assessment and selection of human blastocysts after in vitro fertilization. NPJ Digital Medicine 2(1):1–9
Curchoe CL, Bormann CL (2019) Artificial intelligence and machine learning for human reproduction and embryology presented at ASRM and ESHRE 2018. J Assist Reprod Genet 36(4):591–600
Inhorn MC, Patrizio P (2015) Infertility around the globe: new thinking on gender, reproductive technologies and global movements in the 21st century. Hum Reprod Update 21(4):411–426
Beam AL, Kohane IS (2018) Big data and machine learning in health care. JAMA 319(13):1317–1318
Uyar A, Bener A, Ciray HN (2015) Predictive modeling of implantation outcome in an in vitro fertilization setting: an application of machine learning methods. Med Decis Making 35(6):714–725
Crown WH (2015) Potential application of machine learning in health outcomes research and some statistical cautions. Value in Health 18(2):137–140
Qiu J, Li P, Dong M, Xin X, Tan J (2019) Personalized prediction of live birth prior to the first in vitro fertilization treatment: a machine learning method. J Transl Med 17(1):1–8
Babitha, M. Survey on the machine learning techniques used in IVF treatment to improve the success rate (2019)
Rodríguez-Pérez R, Bajorath J (2019) Interpretation of compound activity predictions from complex machine learning models using local approximations and Shapley values. J Med Chem 63(16):8761–8777
Zhao Y-Y, Yu Y, Zhang X-W (2018) Overall blastocyst quality, trophectoderm grade, and inner cell mass grade predict pregnancy outcome in euploid blastocyst transfer cycles. Chin Med J 131(11):1261–1267
Lai I et al (2020) Transfers of lower quality embryos based on morphological appearance result in appreciable live birth rates: a Canadian center’s experience. F&S Reports 1(3):264–269
Kühnlein M, Appelhans T, Thies B, Nauss T (2014) Improving the accuracy of rainfall rates from optical satellite sensors with machine learning-a random forests-based approach applied to MSG SEVIRI. Remote Sens Environ 141:129–143
Brugo-Olmedo S, Chillik C, Kopelman S (2001) Definition and causes of infertility. Reprod Biomed Online 2(1):173–185
Brandy E et al (2015) Births: final data for 2014. Nat Vital Stat Rep 64:1–64
De la Rochebrochard E, Thonneau P (2003) Paternal age \(\ge\) 40 years: an important risk factor for infertility. Am J Obstet Gynecol 189(4):901–905
Rossi AC, Prefumo F (2016) The effects of surgery for endometriosis on pregnancy outcomes following in vitro fertilization and embryo transfer: a systematic review and meta-analysis. Arch Gynecol Obstet 294(3):647–655
Murta M et al (2018) Endometriosis does not affect live birth rates of patients submitted to assisted reproduction techniques: analysis of the Latin American network registry database from 1995 to 2011. J Assist Reprod Genet 35(8):1395–1399
Sharma S et al (2019) Does presence of adenomyosis affect reproductive outcome in IVF cycles? A retrospective analysis of 973 patients. Reprod Biomed Online 38(1):13–21
Ballester M et al (2012) Cumulative pregnancy rate after ICSI-IVF in patients with colorectal endometriosis: results of a multicentre study. Hum Reprod 27(4):1043–1049
Ferrero S et al (2015) Second surgery for recurrent unilateral endometriomas and impact on ovarian reserve: a case-control study. Fertil Steril 103(5):1236–1243
Maignien C et al (2017) Prognostic factors for assisted reproductive technology in women with endometriosis-related infertility. Am J Obstet Gynecol 216(3):280-e1
Vaegter KK et al (2017) Which factors are most predictive for live birth after in vitro fertilization and intracytoplasmic sperm injection (IVF/ICSI) treatments? Analysis of 100 prospectively recorded variables in 8,400 IVF/ICSI single-embryo transfers. Fertil Steril 107(3):641–648
Choe SA et al (2011) Symmetry in number of retrieved oocytes between two ovaries: a possible predictor of in vitro fertilization outcome. Gynecol Endocrinol 27(12):997–1000
Sunkara SK et al (2011) Association between the number of eggs and live birth in IVF treatment: an analysis of 400 135 treatment cycles. Hum Reprod 26(7):1768–1774
Steward RG et al (2014) Oocyte number as a predictor for ovarian hyperstimulation syndrome and live birth: an analysis of 256,381 in vitro fertilization cycles. Fertil Steril 101(4):967–973
Timeva T et al (2006) Correlation between number of retrieved oocytes and pregnancy rate after in vitro fertilization/intracytoplasmic sperm infection. Sci World J 6:686–690
Bals-Pratsch M et al (2010) Extended analyses of the German IVF registry (DIR): andrological aspects, medical-economical assumptions related to the shift from IVF to ICSI and stimulation with gonadotropins. Journal für Reproduktionsmedizin und Endokrinologie-Journal of Reproductive Medicine and Endocrinology 7(1):40–44
Gambadauro P, Navaratnarajah R (2015) Reporting of embryo transfer methods in IVF research: a cross-sectional study. Reprod Biomed Online 30(2):137–143
Brown, J., Buckingham, K., Buckett, W. & Abou-Setta, A. M. Ultrasound versus ’clinical touch’ for catheter guidance during embryo transfer in women. Cochrane database of systematic reviews (3) (2016)
Ren X et al (2016) Effect of catheter choice during embryo transfer on the clinical outcome of in vitro fertilization-embryo transfer. Beijing da xue xue bao. Yi xue ban= Journal of Peking University. Health Sciences 48(5):905–909
Author information
Authors and Affiliations
Contributions
Conception: NCNB, FMR, KBG. Planning: NCNB, FANP, FMR, IKDC, KBG. Analyzing: NCNB, GZC, RGP, WMJ. Writing: NCNB, FMR, IKDC, KBG, GZC, RGP
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
C. N. Barreto, N., Castro, G.Z., Pereira, R.G. et al. Predicting in vitro fertilization success in the Brazilian public health system: a machine learning approach. Med Biol Eng Comput 60, 1851–1861 (2022). https://doi.org/10.1007/s11517-022-02569-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02569-1