Abstract
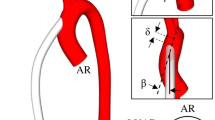
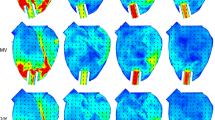
This article describes the numerical efforts made to investigate the influence of a left ventricular assist device (LVAD) on the patient-specific left heart’s hemodynamics. Two different computational geometries with left heart have been simulated over the entire cardiac cycle (case 1: healthy heart without LVAD and case 2: diseased heart with LVAD). The blood flow was simulated by implementing Bird-Carreau non-Newtonian model. Simulation results show that implantation of LVAD pump imparts major influence on the hemodynamics of the heart; it also provides a cardiac output of 4.87 L/min even at the diastolic phase. Furthermore, post LVAD implantation, approximately eight times more wall shear stress, is noticed at the aorta during the ventricular systole. In particular, major changes in the fluidics are observed inside the aortic region. A possibility of flow stagnation is noticed near the aortic root during the diastolic phase due to the bisection of incoming bloodstreams from the outflow graft. The flow characteristics of the LVAD pump are also observed to be significantly different from the idealized simulations (idealized tubular inlet situation). The observation of this study can help in understanding post-implant critical hemodynamic issues due to pump performance and its subsequent impact on the heart.
Graphical abstract
A simulation approach-based study has been performed to investigate the influence of LVAD on the hemodynamics of a heart. A 3D computational model of a patient-specific heart has been created from CT scan datasets for diastole and systole phases (a). An axial flow blood pump has been implanted computationally into the left heart (b). The implanted blood pump enhances the cardiac output and elevates shear generation (c) and (d).
















Similar content being viewed by others
References
Ambrosy AP, Fonarow GC, Butler J et al (2014) The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol 63(12):1123–1133
Trivedi JR, Cheng A, Singh R, Williams ML, Slaughter MS (2014) Survival on the heart transplant waiting list: impact of continuous flow left ventricular assist device as bridge to transplant. Ann Thorac Surg 98:830–834
InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Types of heart failure. 2018 Jan 25. Available from: https://www.ncbi.nlm.nih.gov/books/NBK481485/
Sen A, Larson JS, Kashani KB et al (2013) Mechanical circulatory assist devices: a primer for critical care and emergency physicians. Crit Care 20(1):153
Stöhr EJ, McDonnell BJ, Colombo PC, Willey JZ (2019) CrossTalk proposal: blood flow pulsatility in left ventricular assist device patients is essential to maintain normal brain physiology. J Physiol 597:353–356
Pozzi M, Giraud R, Tozzi P et al (2015) Long-term continuous-flow left ventricular assist devices (LVAD) as bridge to heart transplantation. J Thorac Dis 7(3):532–542. https://doi.org/10.3978/j.issn.2072-1439.2015.01.45
Cheng A, Williamitis CA, Slaughter MS (2014) Comparison of continuous-flow and pulsatile-flow left ventricular assist devices: is there an advantage to pulsatility? Ann Cardiothorac Surg 3(6):573–581. https://doi.org/10.3978/j.issn.2225-319X.2014.08.24
Kannojiya V, Das AK, Das PK (2021) Comparative assessment of different versions of axial and centrifugal LVADs: a review. Artif Organs Early Access. https://doi.org/10.1111/aor.13914
Su B, Kabinejadian F, Phang HQ, Kumar GP, Cui F, Kim S et al (2015) Numerical modeling of intraventricular flow during diastole after implantation of BMHV. PLoS ONE 10(5):e0126315. https://doi.org/10.1371/journal.pone.0126315
Seo JH, Vedula V, Abraham T, Lardo AC, Dawoud F, Luo H, Mittal R (2014) Effect of the mitral valve on diastolic flow patterns. Phys Fluids 26:121901
Lantz J, Gupta V, Henriksson L, Karlsson M, Persson A, Carlhäll CJ, Ebbers T (2019) Impact of pulmonary venous inflow on cardiac flow simulations: comparison with in vivo 4d flow MRI. Ann Biomed Eng 47(2):413–424
Lantz J, Henriksson L, Persson A, Karlsson M, Ebbers T (2016) Patient-specific simulation of cardiac blood flow from high-resolution computed tomography. J Biomech Eng 138(12):121004-1–9. https://doi.org/10.1115/1.4034652
Jahanzamin J, Fatouraee N, Moghaddam AN (2019) Effect of turbulent models on left ventricle diastolic flow patterns simulation. Comput Methods Biomech Biomed Eng 22(15):1229–1238
Wiegmann L, Boes S, de ZeLicourt DD, Thamsen B, Schmid Daners M, Meboldt M et al (2018) Blood pump design variations and their influence on hydraulic performance and indicators of hemocompatibility. Ann Biomed Eng 46:417–428
Heck LM, Yen A, Snyder TA, O’Rear EA, Papavassiliou V (2017) Flowfield simulations and hemolysis estimated for the food and drug administration critical path initiative centrifugal blood pump. Artif Organs 41:E129–E140
Kannojiya V, Das AK, Das PK (2020) Numerical simulation of centrifugal and hemodynamically levitated LVAD for performance improvement. Artif Organs 44(2):E1–E19
Yu J, Zhang X (2016) Hydrodynamic and hemolysis analysis on distance and clearance between impeller and diffuser of axial blood pump. J Mech Med Biol 16(1):1650014
Good BC, Manning KB (2020) Computational modeling of the food and drug administration’s benchmark centrifugal blood pump. Artif Organs 44(7):E263–E276
Karmonik C, Partovi S, Loebe M, Schmack B, Weymann A, Lumsden AB, Karck M, Ruhparwar A (2014) Computational fluid dynamics in patients with continuous-flow left ventricular assist device support show hemodynamic alterations in the ascending aorta. J Thorac Cardiovasc Surg 147(4):1326-1333.e1. https://doi.org/10.1016/j.jtcvs.2013.09.069
Aliseda A, Chivukula VK, Mcgah P, Prisco AR, Beckman JA, Garcia GJ, Mokadam NA, Mahr C (2017) LVAD outflow graft angle and thrombosis risk. ASAIO J Jan/Feb 63(1):14–23. https://doi.org/10.1097/MAT.0000000000000443
Kasinpila P, Kong S, Fong R, Shad R, Kaiser AD, Marsden AL, Woo YJ, Hiesinger W (2020) Use of patient-specific computational models for optimization of aortic insufficiency after implantation of left ventricular assist device. J Thorac Cardiovasc Surg 15:S0022–5223(20)31173–9. doi: https://doi.org/10.1016/j.jtcvs.2020.04.164.
Aigner P, Schweiger M, Fraser K et al (2020) Ventricular flow field visualization during mechanical circulatory support in the assisted isolated beating heart. Ann Biomed Eng 48:794–804. https://doi.org/10.1007/s10439-019-02406-x
Wang Y, Wang J, Peng J, Huo M, Yang Z, Giridharan GA, Luan Y, Qin K (2021) Effects of a short-term left ventricular assist device on hemodynamics in a heart failure patient-specific aorta model: a CFD study. Front Physiol 12:1518
Ghodrati M, Maurer A, Schlöglhofer T, Khienwad T, Zimpfer D, Beitzke D, Zonta F, Moscato F, Schima H, Aigner P (2020) The influence of left ventricular assist device inflow cannula position on thrombosis risk. Artif Organs 44(9):939–946
Su B, Wang X, Kabinejadian F, Chin C, Le TT, Zhang JM (2019) Effects of left atrium on intraventricular flow in numerical simulations. Comput Biol Med 106:46–53
Kannojiya V, Das AK, Das PK (2020) Proposal of hemodynamically improved design of an axial flow blood pump for LVAD. Med Biol Eng Comput 58(2):401–418
GiersiepenM WLJ, Opitz R, Reul H (1990) Estimation of shear stress-related blood damage in heart valve prostheses in vitro comparison of 25 aortic valves. Int J Artif Organs 13(5):300–306
Taskin ME, Fraser KH, Zhang T, Gellman B, Fleischli A, Dasse KA et al (2010) Computational characterization of flow and hemolytic performance of the UltraMag blood pump for circulatory support. Artif Organs 34:1099–1113
Faghig MM, Sharp MK (2016) Extending the power-law hemolysis model to complex flows. J Biomech Eng 138:124504–124511
Caruso MV, Gramigna V, Rossi M, Serraino GF, Renzulli A, Fragomeni G (2015) A computational fluid dynamics comparison between different outflow graft anastomosis locations of left ventricular assist device (LVAD) in a patient-specific aortic model. Int J Numer Method Biomed Eng. 31(2)
Goldstein DJ, Oz MC, Rose EA (1998) Implantable left ventricular assist devices. N Eng J Med 339(21):1522–1533
Dahl SK, Thomassen E, Hellevik LR et al (2012) Impact of pulmonary venous locations on the intra-atrial flow and the mitral valve plane velocity profile. Cardiovasc Eng Tech 3:269–281
Sun A, Zhao B, Ma K, Zhou Z, He L, Li R, Yuan C (2017) Accelerated phase contrast flow imaging with direct complex difference reconstruction. Magn Reson Med 77:1036–1048
Ahmad Bakir A, Al Abed A, Stevens MC, Lovell NH, Dokos S (2018) A multiphysics biventricular cardiac model: simulations with a left-ventricular assist device. Front Physiol. 9:1259. https://doi.org/10.3389/fphys.2018.01259 (Published 2018 Sep 11)
Doost SN, Zhong L, Su B, Morsi YS (2016) The numerical analysis of non-Newtonian blood flow in human patient-specific left ventricle. Comput Methods Programs Biomed 127:232–247
Kannojiya V, Das AK, Das PK (2021) Simulation of blood as fluid: a review from rheological aspects. IEEE Rev Biomed Eng 14:327–341
Khan M, Sardar H, Gulzar MM, Alshomrani AS (2018) On multiple solutions of non-Newtonian Carreau fluid flow over an inclined shrinking sheet. Results Phys 8:926–932
Cho YI, Kensey KR (1991) Effects of the non-Newtonian viscosity of blood on flows in a diseased arterial vessel Part 1: Steady flows. Biorheology 28(3–4):241–262. https://doi.org/10.3233/bir-1991-283-415
Johnston BM, Johnston PR, Corney S, Kilpartrick D (2004) Non-Newtonian blood flow in human right coronary arteries: steady state simulations. J Biomech 37:709–720
Mamun K, Rahman MM, Akhter MN, Ali M (2006) Physiological non-Newtonian blood flow through single stenosed artery. AIP Conf Proc. 2006;1754, Art. no. 040001
Grigoriadis GI, Sakellarios AI, Kosmidou I, Naka KK, Ellis C, Michalis LK, Fotiadis DI (2020) Wall shear stress alterations at left atrium and left atrial appendage employing abnormal blood velocity profiles. Annu Int Conf IEEE Eng Med Biol Soc. 2565–2568.
Dean Vucinic TY, Aksenov AA (2016) Human heart blood flow simulations based on CFD Int. J Fluid Heat Transfer 1:15–34
Sang X, Zhou X (2017) Investigation of hydraulic performance in an axial-flow blood pump with different guide vane outlet angle. Adv Mech Eng 9(8):1–11
Bensalah ZM, Bollache E, Kachenoura N et al (2012) Ascending aorta backward flow parameters estimated from phase-contrast cardiovascular magnetic resonance data: new indices of arterial aging. J Cardiovasc Magn Reson 14:P128. https://doi.org/10.1186/1532-429X-14-S1-P128
Leeuwenburgh BP, Helbing WA, Steendijk P, Schoof PH, Baan J (2003) Effects of acute left ventricular unloading on right ventricular function in normal and chronic right ventricular pressure-overloaded lambs. J Thorac Cardiovasc Surg 125:481–490
Callaghan FM, Grieve SM (2018) Normal patterns of thoracic aortic wall shear stress measured using four-dimensional flow MRI in a large population. Am J Physiol Heart Circ Physiol 315(5):H1174–H1181. https://doi.org/10.1152/ajpheart.00017.2018
De Wachter DS, Verdonck PR, Verhoeven RF, Hombrouckx RO (1996) Red cell injury assessed in a numericalmodel of a peripheral dialysis needle. ASAIO J 42:524–529
Etli M, Canbolat G, Karahan O et al (2021) Numerical investigation of patient-specific thoracic aortic aneurysms and comparison with normal subject via computational fluid dynamics (CFD). Med Biol Eng Comput 59:71–84
Sacco F, Paun B, Lehmkuhl O, Iles TL, Iaizzo PA, Houzeaux G, Vázquez M, Butakoff C, Aguado-Sierra J (2018) Left ventricular trabeculations decrease the wall shear stress and increase the intra-ventricular pressure drop in CFD simulations. Front Physiol 30(9):458
Lopes D, Puga H, Teixeira JC, Teixeira SF (2019) Influence of arterial mechanical properties on carotid blood flow: comparison of CFD and FSI studies. Int J Mech Sci 160:209–218
Torii R, Wood NB, Hadjiloizou N, Dowsey AW, Wright AR, Hughes AD et al (2009) Fluid–structure interaction analysis of a patient-specific right coronary artery with physiological velocity and pressure waveforms. Commun Numer Meth En 25(5):565–580
Acknowledgements
This research work was supported by the Ministry of Human Resource Development (MHRD) and Indian Council of Medical Research (ICMR) under the IMPRINT scheme (award number 3-18/2015-TSI).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Kannojiya, V., Das, A.K. & Das, P.K. Effect of left ventricular assist device on the hemodynamics of a patient-specific left heart. Med Biol Eng Comput 60, 1705–1721 (2022). https://doi.org/10.1007/s11517-022-02572-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02572-6