Abstract
Variability in swallowing electromyography (EMG) has been reported to occur due to individual differences, even in studies with appropriate control of factors affecting EMG such as food type, properties, and posture. The increased variability broadens the confidence intervals of measures obtained from EMG, such as time and amplitude, and makes it difficult to detect differences in muscle activity. This makes it impossible to detect slight changes in swallowing function at an early stage, which is required for clinical examination. In this study, we focused on the tipper type and dipper type of oral swallows, which differ in the timing of muscle activity. The frequency of occurrence of both types varies between participants, and both types could occur in the same participant. In this study, we measured swallowing EMG wherein participants were instructed to swallow with a tipper and a dipper. The results showed that there was a significant difference in the between-participant duration between these two types of swallows. Within-participant variability was significantly lower in the tipper-dipper instruction condition compared to the baseline condition, which assumed a mixture of tipper-dipper swallowing. These results demonstrate that instructions on swallowing method are effective in improving the reproducibility of EMG.
Graphical abstract





Similar content being viewed by others
References
Vaiman M, Eviatar E (2009) Surface electromyography as a screening method for evaluation of dysphagia and odynophagia. Head Face Med 5(9):9. https://doi.org/10.1186/1746-160X-5-9
Vaiman M (2007) Standardization of surface electromyography utilized to evaluate patients with dysphagia. Head Face Med 3(26):26. https://doi.org/10.1186/1746-160X-3-26
Audag N, Goubau C, Toussaint M, Reychler G (2019) Screening and evaluation tools of dysphagia in adults with neuromuscular diseases: a systematic review. Ther Adv Chronic Dis 10:2040622318821622. https://doi.org/10.1177/2040622318821622
Archer SK, Garrod R, Hart N, Miller S (2013) Dysphagia in duchenne muscular dystrophy assessed objectively by surface electromyography. Dysphagia 28(2):188–198. https://doi.org/10.1007/s00455-012-9429-6
Sakai K, Nakayama E, Rogus-Pulia N, Takehisa T, Takehisa Y, Urayama KY, Takahashi O (2020) Submental muscle activity and its role in diagnosing sarcopenic dysphagia. Clin Interv Aging 15:1991–1999. https://doi.org/10.2147/CIA.S278793
Cosentino G, Alfonsi E, Mainardi L, Alvisi E, Brighina F, Valentino F, Fierro B, Sandrini G, Bertino G, Berlangieri M et al (2017) The importance of the reproducibility of oropharyngeal swallowing in amyotrophic lateral sclerosis. An electrophysiological study. Clin Neurophysiol 128(5):792–798. https://doi.org/10.1016/j.clinph.2017.02.006
Ayuse T, Ayuse T, Ishitobi S, Kurata S, Sakamoto E, Okayasu I, Oi K (2006) Effect of reclining and chin-tuck position on the coordination between respiration and swallowing. J Oral Rehabil 33(6):402–408. https://doi.org/10.1111/j.1365-2842.2005.01586.x
Inagaki D, Miyaoka Y, Ashida I, Ueda K, Yamada Y (2007) Influences of body posture on duration of oral swallowing in normal young adults. J Oral Rehabil 34(6):414–421. https://doi.org/10.1111/j.1365-2842.2007.01737.x
Ono T, Iwata H, Hori K, Tamine K, Kondoh J, Hamanaka S, Maeda Y (2009) Evaluation of tongue-, jaw-, and swallowing-related muscle coordination during voluntarily triggered swallowing. Int J Prosthodont 22(5):493–498
Palmer PM, Luschei ES, Jaffe D, Mcculloch TM (1999) Contributions of individual muscles to the submental surface electromyogram during swallowing. J Speech Lang Hear Res 42(6):1378–1391. https://doi.org/10.1044/jslhr.4206.1378
Vaiman M, Eviatar E, Segal S (2004) Evaluation of normal deglutition with the help of rectified surface electromyography records. Dysphagia 19(2):125–132. https://doi.org/10.1007/s00455-003-0504-x
Lininger M, Riemann BL (2016) Statistical primer for athletic trainers: Using confidence intervals and effect sizes to evaluate clinical meaningfulness. J Athl Train 51(12):1045–1048. https://doi.org/10.4085/1062-6050-51.12.14
Aydogdu I, Kiylioglu N, Tarlaci S, Tanriverdi Z, Alpaydin S, Acarer A, Baysal L, Arpaci E, Yuceyar N, Secil Y et al (2015) Diagnostic value of “dysphagia limit” for neurogenic dysphagia: 17 years of experience in 1278 adults. Clin Neurophysiol 126(3):634–643. https://doi.org/10.1016/j.clinph.2014.06.035
Inagaki D, Miyaoka Y, Ashida I, Yamada Y (2008) Influence of food properties and body posture on durations of swallowing-related muscle activities. J Oral Rehabil 35(9):656–663. https://doi.org/10.1111/j.1365-2842.2008.01866.x
Inagaki D, Miyaoka Y, Ashida I, Yamada Y (2009) Influence of food properties and body position on swallowing-related muscle activity amplitude. J Oral Rehabil 36(3):176–183. https://doi.org/10.1111/j.1365-2842.2008.01927.x
Sakuma T, Kida I (2010) Relationship between ease of swallowing and deglutition-related muscle activity in various postures. J Oral Rehabil 37(8):583–589. https://doi.org/10.1111/j.1365-2842.2010.02084.x
Kohyama K, Sawada H, Nonaka M, Kobori C, Hayakawa F, Sasaki T (2007) Textural evaluation of rice cake by chewing and swallowing measurements on human subjects. Biosci Biotechnol Biochem 71(2):358–365. https://doi.org/10.1271/bbb.60276
Inui R, Mori S, Nakajima T, Lee H, Nishimori T, Tabira K (2012) Influence of neck position on the activity of pharyngeal and neck muscles during swallowing—examination by surface electromyography―. Jpn J Dysphagia Rehabil 16(3):269–275. https://doi.org/10.32136/jsdr.16.3_269 (in Japanese)
Miralles R, Palazzi C, Ormeño G, Giannini R, Verdugo F, Valenzuela S, Santander H (1998) Body position effects on emg activity of sternocleidomastoid and masseter muscles in healthy subjects. Cranio 16(2):90–99. https://doi.org/10.1080/08869634.1998.11746045
Lof GL, Robbins J (1990) Test–retest variability in normal swallowing. Dysphagia 4(4):236–242. https://doi.org/10.1007/BF02407271
Costa MM (2010) Videofluoroscopy: the gold standard exam for studying swallowing and its dysfunction. Arq Gastroenterol 47(4):327–328. https://doi.org/10.1590/S0004-28032010000400001
Gramigna GD (2006) How to perform video-fluoroscopic swallowing studies. GI Motility online
Martin-Harris B, Jones B (2008) The videofluorographic swallowing study. Phys Med Rehabil Clin N Am 19(4):769–785. https://doi.org/10.1016/j.pmr.2008.06.004
Ohmori N, Chikai M, Endo H, Ino S (2017) Experimental investigation of variability in swallowing measurement Proceedings of the human interface symposium, vol 2017 5Tp3–1 (in Japanese)
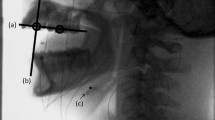
Dodds WJ, Taylor AJ, Stewart ET, Kern MK, Logemann JA, Cook IJ (1989) Tipper and dipper types of oral swallows. AJR Am J Roentgenol 153(6):1197–1199. https://doi.org/10.2214/ajr.153.6.1197
Cook IJ, Dodds WJ, Dantas RO, Kern MK, Massey BT, Shaker R, Hogan WJ (1989) Timing of videofluoroscopic, manometric events, and bolus transit during the oral and pharyngeal phases of swallowing. Dysphagia 4(1):8–15. https://doi.org/10.1007/BF02407397
Sugino S, Taniguchi H, Tsukada T, Ootaki S, Kajii Y, Yamada Y, Inoue M (2007) Effects of food consistency and subject’s posture on the electromyographic activity in the genioglossus muscle in humans. J Jpn Soc Stomatognath Funct 14(1):13–23. https://doi.org/10.7144/sgf.14.13(inJapanese)
Yang Y, Leow LP, Yoon WL, Rickard Liow SJ, Chua KC (2012) Relationship between age and drinking instructions on the modification of drinking behavior. Dysphagia 27(2):210–215. https://doi.org/10.1007/s00455-011-9355-z
Perlman AL, Palmer PM, Mcculloch TM (1985) Vandaele DJ (1999) Electromyographic activity from human laryngeal, pharyngeal, and submental muscles during swallowing. J Appl Physiol 86(5):1663–1669. https://doi.org/10.1152/jappl.1999.86.5.1663
Koyama Y, Ohmori N, Momose H, Kondo E, Yamada SI, Kurita H (2021) Detection of swallowing disorders using a multiple channel surface electromyography sheet: a preliminary study. J Dent Sci 16(1):160–167. https://doi.org/10.1016/j.jds.2020.06.009
Zaretsky E, Pluschinski P, Sader R, Birkholz P, Neuschaefer-Rube C, Hey C (2017) Identification of the most significant electrode positions in electromyographic evaluation of swallowing-related movements in humans. Eur Arch Otorhinolaryngol 274(2):989–995. https://doi.org/10.1007/s00405-016-4288-7
Yokoyama M, Michiwaki Y, Takahashi K, Ozawa M, Akizuki A, Michi K (2000) Analysis of swallowing function using videofluorographic images-basic study for the time analysis-. J Jpn Stomatol Soc 49(1):16–24. https://doi.org/10.11277/stomatology1952.49.16 (in Japanese)
Hori K, Taniguchi H, Hayashi H, Magara J, Minagi Y, Li Q, Ono T, Inoue M (2013) Role of tongue pressure production in oropharyngeal swallow biomechanics. Physiol Rep 1(6):e00167. https://doi.org/10.1002/phy2.167
Nakane A, Tohara H, Ouchi Y, Goto S, Uematsu H (2006) Videofluoroscopic kinesiologic analysis of swallowing: defining a standard plane. J Med Dent Sci 53(1):7–15
Ohmori N, Murasawa C, Aizawa J, Momose H, Koyama Y, Kurita H, Yoshida H, Kamijo M (2017) Noise reduction in swallowing muscle activity measurement based on mixture Gaussian distribution model. J Adv Comp Intell Intell Inform 21(1):109–118. https://doi.org/10.20965/jaciii.2017.p0109
Kouchi M, Mochimaru M (2005) Aist anthropometric database. Natl Inst Adv Ind Sci Technol H16PRO 287
Halaki M, Gi K (2012) Normalization of emg signals: to normalize or not to normalize and what to normalize to? In: Comp Intell Electromyogr Anal Perspect Curr Appl Future Chall 175–194
Kuiken TA, Lowery MM, Stoykov NS (2003) The effect of subcutaneous fat on myoelectric signal amplitude and cross-talk. Prosthet Orthot Int 27(1):48–54. https://doi.org/10.3109/03093640309167976
Sousa AS, Tavares JMR (2012) Surface electromyographic amplitude normalization methods: a review electromyography: new developments, procedures and applications, pp 85–102
Koo TK, Li MY (2016) A guideline of selecting and reporting intraclass correlation coefficients for reliability research. J Chiropr Med 15(2):155–163. https://doi.org/10.1016/j.jcm.2016.02.012
Acknowledgements
The authors would like to thank the participants who participated in the experiments. In addition, the authors wish to thank: Dr. Hidekazu Kaneko, who is a Senior Researcher at the National Institute of Advanced Industrial Science and Technology in Japan; Dr. Syuji Ishiguro, who is the Division Director of the Nagano Prefecture General Industrial Technology Center in Japan; and Dr. Yoshito Koyama and Dr. Hiroshi Kurita from Shinshu University in Japan for their valuable opinions. Finally, we would like to acknowledge Mr. Tomoki Sawano and Ms. Aasahi Koyama for their valuable research support.
Funding
This study was supported by the Strategic Information and Communications R&D Promotion Programme (SCOPE), the Ministry of Internal Affairs and Communications Japan, and the JSPS KAKENHI grant numbers JP17H00755, 19K12887, 20H04567, and 20K11929.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The institutions of the authors (Nagano Prefecture and SKINOS) have patents that are issued and pending. The authors declare no competing interests other than the above.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ohmori, N., Watanabe, S., Momose, H. et al. Investigation of variation factors in EMG measurement of swallowing: instruction can improve EMG reproducibility. Med Biol Eng Comput 60, 2825–2840 (2022). https://doi.org/10.1007/s11517-022-02590-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02590-4