Abstract
Congenital tracheal stenosis (CTS) with unilateral pulmonary agenesis (UPA) is characterized by the absence of one or both lungs in the hemithorax and is often associated with airway distortion. Some UPA patients have high mortality and morbidity even postoperatively, and it remains unclear whether surgery increases the energy flux needed to drive airflow. Here, we used pre- and postoperative patient-specific airway models to numerically investigate tracheal flow in patients with CTS, especially flow associated with right UPA (CTS-RUPA). Airflow was simulated with the large-eddy model, and energy flux was investigated to quantify airway performance and the contribution of surgical intervention. Although energy flux decreased postoperatively, clinical respiratory status did not improve. Standard surgical intervention for CTS, which expands the minimal cross-sectional area, decreased energy flux, i.e., improved airway performance. The simulation also included artificial airways with a straightened bend or reduced tracheal lumen roughness. The numerical results clearly showed interindividual differences in the percent reduction of energy flux caused by straightening the tracheal bend versus correcting tracheal lumen roughness. Although this study was limited to small sample size, these numerical results indicated that energy flux alone is insufficient to evaluate breathing performance in patients with CTS-RUPA but it can be used to estimate airway performance.
Graphical abstract







Similar content being viewed by others
Abbreviations
- CTS:
-
Congenital tracheal stenosis
- UPA:
-
Unilateral pulmonary agenesis
- RUPA:
-
Right unilateral pulmonary agenesis
- LUPA:
-
Left unilateral pulmonary agenesis
- LES:
-
Large-eddy simulation
- CFD:
-
Computational fluid dynamics
- CT:
-
Computed tomography
- ρ :
-
Air density
- µ :
-
Viscosity
- D :
-
Average diameter of trachea
- D in :
-
Inlet diameter
- U in :
-
Inlet velocity
- Q in :
-
Flow rate
- P in :
-
Pressure in the inlet
- P out :
-
Pressure in the outlet
- L :
-
Length of the line at the center of the real airway
- L 0 :
-
Euclidean distance from the start to the end points of extracted tracheas
- A :
-
Cross-sectional area
- A min :
-
The minimum cross-sectional area
- \(\sigma\) A :
-
Standard deviation of the cross-sectional area
- E T :
-
Energy flux
References
Antón-Pacheco JL, Cano I, Comas J, Galletti L, Polo L, García A, López M, Cabezalí D (2006) Management of congenital tracheal stenosis in infancy. Eur J Cardio-Thorac Surg 29:991–996. https://doi.org/10.1016/j.ejcts.2005.12.061
Bates AJ, Cetto R, Doorly DJ, Schroter RC, Tolley NS, Comerford A (2016) The effects of curvature and constriction on airflow and energy loss in pathological tracheas. Respir Physiol Neurobiol 234:69–78. https://doi.org/10.1016/j.resp.2016.09.002
Bates AJ, Comerford A, Cetto R, Schroter RC, Tolley NS, Doorly DJ (2016) Power loss mechanisms in pathological tracheas. J Biomech 49:2187–2192. https://doi.org/10.1016/j.jbiomech.2015.11.033
Berdon WE, Baker DH, Wung JT, Chrispin A, Kozlowski K, de Silva M, Bales P, Alford B (1984) Complete cartilage-ring tracheal stenosis associated with anomalous left pulmonary artery: the ring sling complex. Radiology 152:57–64. https://doi.org/10.1148/radiology.152.1.6729137
Berger SA, Talbot L, Yao L-S (1983) Flow in curved pipes. Annu Rev Fluid Mech 15:461–512. https://doi.org/10.1146/annurev.fl.15.010183.002333
Booth JB, Berry CL (1967) Unilateral pulmonary agenesis. Arch Dis Child 42:361–374. https://doi.org/10.1136/adc.42.224.361
Brouns M, Jayaraju ST, Lacor C, Mey JD, Noppen M, Vincken W, Verbanck S (2007) Tracheal stenosis: a flow dynamics study. J Appl Physiol 103:1178–1184. https://doi.org/10.1152/japplphysiol.01063.2006
Chou A-K, Huang S-C, Chen S-J, Huang P-M, Wang J-K, Wu M-H, Chen Y-S, Chang C-I, Chiu I-S, Wu E-T (2007) Unilateral lung agenesis–detrimental roles of surrounding vessels. Pediatr Pulmonol 42:242–248. https://doi.org/10.1002/ppul.20561
Clements JA, Brown ES, Johnson RP (1958) Pulmonary surface tension and the mucus lining of the lungs: some theoretical considerations. J Appl Physiol 12:262–268. https://doi.org/10.1152/jappl.1958.12.2.262
Davis PJ, Cladis FP (2016) Smith’s anesthesia for infants and children, 9th edn. Elsevier, Philadelphia
Donati F, Figueroa CA, Smith NP, Lamata P, Nordsletten DA (2015) Non-invasive pressure difference estimation from PC-MRI using the work-energy equation. Med Image Analysis 26:159–172. https://doi.org/10.1016/j.media.2015.08.012
Ford S, Calvert J (2008) Adaptation for life: a review of neonatal physiology. Anaesth Intensive Care 9:93–98. https://doi.org/10.1016/j.mpaic.2014.01.002
Goldsmith JP, Karothin EH, Martin K, Gautham S (2016) Assisted ventilation of the neonate: evidence-based approach to newborn respiratory care, 6th edn. Elsevier, Philadelphia
Grinnan DC, Truwit JD (2005) Clinical review: respiratory mechanics in spontaneous and assisted ventilation. Crit Care 9:472–484. https://doi.org/10.1186/cc3516
Grotberg JB (2001) Respiratory fluid mechanics and transport processes. Ann Rev Biomed Eng 3:421–457. https://doi.org/10.1146/annurev.bioeng.3.1.421
Grotberg JB (2011) Respiratory fluid mechanics. Phys Fluids 23:021301. https://doi.org/10.1063/1.3517737
Hasegawa T, Oshima Y, Maruo A, Matsuhisa H, Yokoi A, Okata Y, Nishijima E, Yamaguchi M (2014) Pediatric cardiothoracic surgery in patients with unilateral pulmonary agenesis or aplasia. Ann Thorac Surg 97:1652–1658. https://doi.org/10.1016/j.athoracsur.2013.11.022
Herrera P, Caldarone C, Forte V, Campisi P, Holtby H, Chait P, Chiu P, Cox P, Yoo S-J, Manson D, Kim PCW (2007) The current state of congenital tracheal stenosis. Pediatr Surg Int 23:1033–1044. https://doi.org/10.1007/s00383-007-1945-3
Hewitt RJ, Butler CR, Maughan EF, Elliott MJ (2016) Congenital tracheobronchial stenosis. Semin Pediatr Surg 25:144–149. https://doi.org/10.1053/j.sempedsurg.2016.02.007
Hofferberth SC, Watters K, Rahbar R, Fynn-Thompson F (2015) Management of congenital tracheal stenosis. Pediatrics 136:e660–e669. https://doi.org/10.1542/peds.2014-3931
Ismail M, Comerford A, Wall WA (2013) Coupled and reduced dimensional modeling of respiratory mechanics during spontaneous breathing. Int J Numer Meth Biomed Engng 29:1285–1305. https://doi.org/10.1002/cnm.2577
Liu CH, Niranjan SC, Clark JW Jr, San KY, Zwischenberger JB, Bidani A (1998) Airway mechanics, gas exchange, and blood flow in a nonlinear model of the normal human lung. J Appl Physiol 84:1447–1469. https://doi.org/10.1152/jappl.1998.84.4.1447
Maltz DL, Nadas AS (1968) Agenesis of the lung: presentation of eight new cases and review of the literature. Pediatrics 42:175–188. https://doi.org/10.1542/peds.42.1.175
Malvè M, Chandra S, López-Villalobos JL, Finol EA, Ginel A, Doblaré M (2013) CFD analysis of the human airways under impedance-based boundary conditions: application to healthy, diseased and stented trachea. Comput Methods Biomech Biomed Eng 16:198–216. https://doi.org/10.1080/10255842.2011.615743
Menter FR (1994) Two-equation eddy-viscosity turbulence models for engineering applications. AIAA J 32:1598–1605. https://doi.org/10.2514/3.12149
Mimouni-Benabu O, Meister L, Giordano J, Fayoux P, Loundon N, Triglia JM, Nicollas R (2012) A preliminary study of computer assisted evaluation of congenital tracheal stenosis: a new tool for surgical decision-making. Int J Pediatr Otorhinolaryngol 76:1552–1557. https://doi.org/10.1016/j.ijporl.2012.07.009
Morita K, Maeda K, Yabe K, Oshima Y (2017) Management of congenital tracheal stenosis in the neonatal period. Pediatr Surg Int 33:1059–1063. https://doi.org/10.1007/s00383-017-4137-9
Pedley TJ (1977) Pulmonary fluid dynamics. Annu Rev Fluid Mech 9:229–274. https://doi.org/10.1146/annurev.fl.09.010177.001305
Qi S, Li Z, Yue Y, van Triest HJW, Kang Y (2014) Computational fluid dynamics simulation of airflow in the trachea and main bronchi for the subjects with left pulmonary artery sling. BioMed Eng OnLine 13:85. https://doi.org/10.1186/1475-925X-13-85
Sul B, Altes T, Ruppert K, Qing K, Hariprasad DS, Morris M, Reifman J, Wallqvist A (2019) Dynamics of the tracheal airway and its influences on respiratory airflows: an exemplar study. J Biomech Eng 141:111009. https://doi.org/10.1115/1.4043723
Shih TH, Zhu J, Lumley JL (1995) A new Reynolds stress algebraic equation model. Comput Methods Appl Mech Engrg 125:287–302. https://doi.org/10.1016/0045-7825(95)00796-4
Shih TH, Liou WW, Shabbir A, Yang Z, Zhu J (1995) A new k-ϵ eddy viscosity model for high reynolds number turbulent flows. Comput Fluids 24:227–238. https://doi.org/10.1016/0045-7930(94)00032-T
Takeishi N, Miki T, Otani T, Ii S, Morita K, Wada S (2019) Fluid dynamic assessment of tracheal flow in infants with congenital tracheal stenosis before and after surgery. Med Biol Eng Comput 57:837–847. https://doi.org/10.1007/s11517-018-1928-7
Tsugawa C, Nishijima E, Muraji T, Satoh S, Takamizawa S, Yamaguchi M, Yoshimura N, Oka S, Kimura K (2003) Tracheoplasty for long segment congenital tracheal stenosis: analysis of 29 patients over two decades. J Pediatr Surg 38:1703–1706. https://doi.org/10.1016/j.jpedsurg.2003.08.037
Weber TR, Connors RH, Tracy TFJ (1991) Congenital tracheal stenosis with unilateral pulmonary agenesis. Ann Surg 213:70–74. https://doi.org/10.1097/00000658-199101000-00012
Xiao Q, Cetto R, Doorly DJ, Bates AJ, Rose JN, McIntyre C, Comerford A, Madani G, Tolley NS, Schroter R (2020) Assessing changes in airflow and energy loss in a progressive tracheal compression before and after surgical correction. Ann Biomed Eng 48:822–833. https://doi.org/10.1007/s10439-019-02410-1
Acknowledgements
This research was supported by JSPS KAKENHI Grant Numbers JP19H01175 and JP20H04504; by the Keihanshin Consortium for Fostering the Next Generation of Global Leaders in Research (K-CONNEX), established by the Human Resource Development Program for Science and Technology; and by MEXT as “Priority Issue on Post-K computer (Supercomputer Fugaku)” (Integrated Computational Life Science to Support Personalized and Preventive Medicine) (Project ID:hp190187). N. T. thanks Dr. S. Ii, Dr. N. Yokoyama, and Dr. T. Otani for helpful discussions.
Author information
Authors and Affiliations
Contributions
S.K., K.T., and N.H. performed the experiments; N.T., S.K., K.T., and N.H. analyzed the data; N.T., and K.M. interpreted the results of experiments; N.T. prepared the figures; N.T. drafted the manuscript; N.T. edited and revised the manuscript; N.T., S.K., K.T., N.H., K.M., and S.W. approved the final version of manuscript; and N.T. conceived and designed the research.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix
Airflows in RUPA and normal subjects
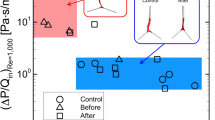
We preliminarily checked the difference in energy flux ET obtained with the LES, realizable k-ε, and SST k-ω turbulence models. Figure
a Airway models for patient P6 before and after surgery (left and right, respectively; straight tubes at the inlet/outlet are not shown); this patient was diagnosed with right lung agenesis without CTS. The models are not to scale and are also rotated for illustrative purposes. b The cross-sectional area A of the trachea is shown as a function of the distance from the inlet of the real airway both preoperatively (solid black line) and postoperatively (solid red line). c Comparison of energy flux ET in P6 before and after surgery, obtained with different turbulence models: LES, realizable k-ε, and k-ω SST models
7 shows the calculated ET obtained with these models before and after surgery in a patient (P6) diagnosed with right lung agenesis without CTS, i.e., tracheal cartilage rings were the same as those in healthy subjects. Since P6 was not diagnosed with CTS, the data was not included in the aforementioned results for 5 patients (P1–P5). Although we could not find significant differences in ET among the three models at least in this patient, all simulations in this study were performed using the LES model, which is higher fidelity than the other two models. Note that P6 was in good prognosis and did not undergo repeat surgery.
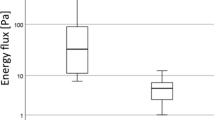
Instead of model validation using, e.g., a lung phantom or microfluidics, we further simulated airflows in five healthy controls (C1–C5) with an average age of seven months. The definition of the target area was from just under the larynx to just below the tracheal bifurcation, with a length of approximately 45–60 mm. One of five normal airway models was shown in Fig.
a One of the normal subject airway models (C1–C5). Straight tubes are attached to the inlet and two outlets of real airways, which are colored red. b The energy flux ET is shown as box plots (five normal subjects, five preoperative patients, and four postoperative patients). The data of each subject are displayed as circles. c ET as a function of the minimum cross-sectional area Amin. The results of five normal controls and P6 were also displayed. The dashed line is the approximation curve same as in Fig. 4b, where data of P1–P5 was only used
8a, where straight tubes with 50 mm length to the inlet and two outlets of real airways were also visualized. Even though normal subject airway models include carina, the median value of ET (90.6 Pa) in healthy controls was smaller than those in CTS-RUPA (140.8 Pa) as shown in Fig. 8b. The result may indicate that the airway performance of preoperative patients with CTS-RUPA is lower than or almost the same as that of healthy subjects. The relationship between ET and Amin for P6 and five healthy controls were added in Fig. 4b, and the results were summarized in Fig. 8c. Although ET in five controls was well approximated by data of P1–P5, ET in P6Aft was far away from the approximation curve (Fig. 8c). Considering this numerical result and good prognosis of P6, clinical respiratory status in patients with RUPA may be different from those in patients with CTS-RUPA. Further statistical analysis is required, which is however our future study.
Realizable k-ε and SST k-ω turbulence
Governing equations of realizable k-ε and shear stress transport (SST) k-ω turbulence models were described below. The 3D steady Reynolds averaged Navier–Stokes (RANS) equations were commonly considered in those models. Substituting mean and fluctuating components of the flow into an incompressible Navier–Stokes equation, continuity and RANS equations are written as
where \({\overline{u} }_{i}\) and \({u}_{i}\) are the mean and fluctuating velocities, \(\overline{p }\) is the mean pressure, and \({\overline{D} }_{ij}\) is a strain-rate tensor, which is given by
The standard eddy viscosity formulation for incompressible turbulence is
For the realizable k-ε turbulence model, the turbulent kinetic energy k and its rate of dissipation ε come directly from their differential transport equations:
and
where σk and σε are the turbulent Prandtl number for k and ε, respectively. Cε1, Cµ and As were computed by:
The other constants (\({\sigma }_{k}\), \({\sigma }_{\varepsilon }\), \({C}_{\varepsilon 2}\), \({A}_O\)) are determined as \({\sigma }_{k}=1.0\), \({\sigma }_{\varepsilon }=1.2\), \({C}_{\varepsilon 2}=1.9\), \({A}_{O}=4.0\) [31]. More precise descriptions about realizable \(k-\varepsilon\) turbulence model should be referred to [31, 32].
In SST \(k-\omega\) turbulence model, the turbulent kinetic energy k and specific dissipation rate \(\omega (=\varepsilon /k)\) are written as
and
where α1 = 0.31, and \({\beta }^{*}=0.09\) [25]. Each constant \(\varphi\) (\({\sigma }_{k}\), \({\sigma }_{\omega }\), \(\gamma\), \(\beta\)) is given by using the blending function F1, and corresponding constant \({\varphi }_{1}\) and \({\varphi }_{2}\)
where \({\sigma }_{k1}=0.85\), \({\sigma }_{k2}=1\), \({\sigma }_{\omega 1}=0.5\), \({\sigma }_{\omega 2}=0.856\), \({\gamma }_{1}=5/9\), \({\gamma }_{2}=0.44\), β1 = 0.075, and \({\beta }_{2}=0.0828\) [25]. More precise descriptions about SST \(k-\omega\) turbulence model should be referred to [25].
Rights and permissions
About this article
Cite this article
Kageyama, S., Takeishi, N., Harada, N. et al. Airway performance in infants with congenital tracheal stenosis associated with unilateral pulmonary agenesis: effect of tracheal shape on energy flux. Med Biol Eng Comput 60, 2335–2348 (2022). https://doi.org/10.1007/s11517-022-02601-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02601-4