Abstract
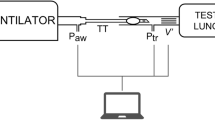
High-flow oxygen therapy using a tracheostomy tube is a promising clinical approach to reduce the work of breathing in tracheostomized patients. Positive end-expiratory pressure (PEEP) is usually applied during oxygen inflow to improve oxygenation by preventing end-expiratory lung collapse. However, much is still unknown about the geometrical effects of PEEP, especially regarding tracheostomy tube connectors (or adapters). Quantifying the degree of end-expiratory pressure (EEP) that takes patient-specific spirometry into account would be useful in this regard, but no such framework has been established yet. Thus, a platform to assess PEEP under respiration was developed, wherein three-dimensional simulation of airflow in a tracheostomy tube connector is coupled with a lumped lung model. The numerical model successfully reflected the magnitude of EEP measured experimentally using a lung phantom. Numerical simulations were further performed to quantify the effects of geometrical parameters on PEEP, such as inlet angles and rate of stenosis in the connector. Although sharp inlet angles increased the magnitude of EEP, they cannot be expected to achieve clinically reasonable PEEP. On the other hand, geometrical constriction in the connector can potentially result in PEEP as obtained with conventional nasal cannulae.
Graphical abstract










Similar content being viewed by others
References
Alzahranya M, Banerjeea A, Salzman G (2014) The role of coupled resistance-compliance in upper tracheobronchial airways under high frequency oscillatory ventilation. Med Eng Phys 36:1593–1604. https://doi.org/10.1016/j.medengphy.2014.08.012
Acute Respiratory Distress Syndrome Network, Brower RG, Matthay MA, Morris A, Schoenfeld D, Thompson BT, Wheeler A (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 4:1301–1308. https://doi.org/10.1056/NEJM200005043421801
Barbini P, Brighenti C, Gnudi G (2006) A simulation study of expiratory flow limitation in obstructive patients during mechanical ventilation. Ann Biomed Eng 34:1879–1889. https://doi.org/10.1007/s10439-006-9213-6
Bräunlich J, Beyer D, Mai D, Hammschmidt S, Seyfarth H-J, Wirtz H (2013) Effects of nasal high flow on ventilation in volunteers, COPD and idiopathic pulmonary fibrosis patients. Respiration 85:319–325. https://doi.org/10.1159/000342027
Brouns M, Jayaraju ST, Lacor C, Mey JD, Noppen M, Vincken W, Verbanck S (2007) Tracheal stenosis: a flow dynamics study. J Appl Physiol 103:1178–1184. https://doi.org/10.1152/japplphysiol.01063.2006
Corley A, Caruana LR, Barnett AG, Tronstad O, Fraser JF (2011) Oxygen delivery through high-flow nasal cannulae increase end-expiratory lung volume and reduce respiratory rate in post-cardiac surgical patients. Br J Anaesth 107:998–1004. https://doi.org/10.1093/bja/aer265
Engoren M, Arslanian-Engoren C, Fenn-Buderer N (2004) Hospital and longterm outcome after tracheostomy for respiratory failure. Chest 125:220–227. https://doi.org/10.1378/chest.125.1.220
Franklin D, Babl FE, Schlapbach LJ, Oakley E, Craig S, Neutze J, Furyk J, Fraser JF, Jones M, Whitty JA, Dalziel SR, Schibler A (2018) A randomized trial of high-flow oxygen therapy in infants with bronchiolitis. N Engl J Med 378:1121–1131. https://doi.org/10.1056/NEJMoa1714855
Fung Y-C (1975) Stress, deformation, and atelectasis of the lung. Circ Res 37:481–496. https://doi.org/10.1161/01.RES.37.4.481
Hashimoto DA, Axtell AL, Auchincloss HG (2020) Percutaneous tracheostomy. N Engl J Med 383:e112. https://doi.org/10.1056/NEJMvcm2014884
Ii S, Wada S (2017) Direct numerical simulation of expiratory crackles: relationship between airway closure dynamics and acoustic fluctuations. J Biomech 50:234–239. https://doi.org/10.1016/j.jbiomech.2016.11.033
Ismail M, Comeford A, Wall WA (2013) Coupled and reduced dimensional modeling of respiratory mechanics during spontaneous breathing. Int J Numer Meth Biomed Eng 29:1285–1305. https://doi.org/10.1002/cnm.2577
Kageyama S, Takeishi N, Harada N, Taniguchi K, Morita K, Wada S (2022) Airway performance in infants with congenital tracheal stenosis associated with unilateral pulmonary agenesis: effect of tracheal shape on energy flux. Med Biol Eng Comput. https://doi.org/10.1007/s11517-022-02601-4
Kim M, Collier GJ, Wild JM, Chung YM (2018) Effect of upper airway on tracheobronchial fluid dynamics. Int J Numer Meth Biomed Eng 34:e3112. https://doi.org/10.1002/cnm.3112
Ma B, Lutchen K (2006) An anatomically based hybrid computational model of the human lung and its application to low frequency oscillatory mechanics. Ann Biomed Eng 34:1691–1704. https://doi.org/10.1007/s10439-006-9184-7
Ma B, Lutchen KR (2008) CFD simulation of aerosol deposition in an anatomically based human large-medium airway model. Ann Biomed Eng 37:271–285. https://doi.org/10.1007/s10439-008-9620-y
Malvè M, Chandra S, López-Villalobos JL, Finol EA, Ginel A, Doblaré M (2013) CFD analysis of the human airways under impedance-based boundary conditions: application to healthy, diseased and stented trachea. Comput Methods Biomech Biomed Eng 16:198–216. https://doi.org/10.1080/10255842.2011.615743
Mead J (1960) Control of respiratory frequency. J Appl Physiol 15:325–336. https://doi.org/10.1152/jappl.1960.15.3.325
Mead J, Takishima T, Leith D (1970) Stress distribution in lungs: a model of pulmonary elasticity. J Appl Physiol 28:596–608. https://doi.org/10.1152/jappl.1970.28.5.596
Meade MO, Cook DJ, Guyatt GH, Slutsky AS, Arabi YM, Cooper DJ, Davies AR, Hand LE, Zhou Q, Thabane L, Austin P, Lapinsky S, Baxter A, Russell J, Skrobik Y, Ronco JJ, Stewart TE, Lung Open Ventilation Study Investigators (2008) Ventilation strategy using low tidal volumes, recruitment maneuvers, and high positive end-expiratory pressure for acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 299:637–645. https://doi.org/10.1001/jama.299.6.637
Milési C, Baleine J, Matecki S, Durand S, Combes C, Novais ARB, Combonie G (2013) Is treatment with a high flow nasal cannula effective in acute viral bronchiolitis? Intensive Care Med 39:1088–1094. https://doi.org/10.1007/s00134-013-2879-y
Moller W, Celik G, Feng S, Bartenstein P, Meyer G, Oliver E, Schmid O, Tatkov S (2015) Nasal high flow clears anatomical dead space in upper airway models. J Appl Physiol 118:1525–1532. https://doi.org/10.1152/japplphysiol.00934.2014
Moller W, Feng S, Domanski U, Franke KJ, Celik G, Bartenstein P, Becker S, Meyer G, Schmid O, Eickelberg O, Tatkov S, Nilius G (2017) Nasal high flow reduces dead space. J Appl Physiol 122:191–197. https://doi.org/10.1152/japplphysiol.00584.2016
Natalini D, Grieco DL, Santantonio MT, Mincione L, Toni F, Anzellotti GM, Eleuteri D, Giannatale PD, Antonelli M, Maggiore SM (2019) Physiological effects of high-flow oxygen in tracheostomized patients. Ann Intensive Care 9:114. https://doi.org/10.1186/s13613-019-0591-y
Papazian L, Corley A, Hess D, Fraser JF, Frat J-P, Guitton C, Jaber S, Maggiore SM, Nava S, Rello J, Ricard J-D, Stephan F, Trisolini R, Azoulay E (2016) Use of high-flow nasal cannula oxygenation in ICU adults: a narrative review. Intensive Care Med 42:1336–1349. https://doi.org/10.1007/s00134-016-4277-8
Parke RL, McGuinness SP (2013) Pressures delivered by nasal high flow oxygen during all phases of the respiratory cycle. Respir Care 58:1621–1624. https://doi.org/10.4187/respcare.02358
Pedley TJ (1977) Pulmonary fluid dynamics. Ann Rev Fluid Mech 9:229–274. https://doi.org/10.1146/annurev.fl.09.010177.001305
Peek GJ, Mugford M, Tiruvoipati R, Wilson A, Allen E, Thalanany MM, Hibbert CL, Truesdale A, Clemens F, Cooper N, Firmin RK, Elbourne D, CESAR trial collaboration (2009) Efficacy and economic assessment of conventional ventilatory support versus extracorporeal membrane oxygenation for severe adult respiratory failure (CESAR): a multicentre randomised controlled trial. Lancet 374:1351–1363. https://doi.org/10.1016/S0140-6736(09)61069-2
Rausch SMK, Martin C, Bornemann PB, Uhlig S, Wall WA (2011) Material model of lung parenchyma based on living precision-cut lung slice testing. J Mech Behav Biomed Mater 4:583–592. https://doi.org/10.1016/j.jmbbm.2011.01.006
Van Rhein T, Alzahrany M, Bajerjee A, Salzman G (2016) Fluid flow and particle transport in mechanically ventilated airways. part I. fluid flow structures. Med Biol Eng Comput 54:1085–1096. https://doi.org/10.1007/s11517-015-1407-3
Sattari S, Eskandari M (2020) Characterizing the viscoelasticity of extra- and intra-parenchymal lung bronchi. J Mech Behav Biomed Mater 110:103824. https://doi.org/10.1016/j.jmbbm.2020.103824
Shih TH, Liou WW, Shabbir A, Yang Z, Zhu J (1995) A new k-ε eddy viscosity model for high reynolds number turbulent flows. Comput Fluids 24:227–238. https://doi.org/10.1016/0045-7930(94)00032-T
Slutsky AS, Ranieri VM (2013) Ventilator-induced lung injury. N Engl J Med 369:2126–2136. https://doi.org/10.1056/NEJMra1208707
Spoletini G, Alotaibi M, Blasi F, Hill NS (2015) Heated humidified high-flow nasal oxygen in adults: mechanisms of action and clinical implications. Chest 148:253–261. https://doi.org/10.1378/chest.14-2871
Stripoli T, Spadaro S, Di mussi R, Volta CA, Trerotoli P, Carlo FD, Iannuzziello R, Sechi F, Pierucci P, Staffieri F, Bruno F, Camporota L, Grasso S (2019) High-flow oxygen therapy in tracheostomized patients at high risk of weaning failure. Ann Intensive Care 9:4. https://doi.org/10.1186/s13613-019-0482-2
Sztrymf B, Messika J, Bertrand F, Hurel D, Leon R, Dreyfuss D, Ricard J-D (2011) Beneficial effects of humidified high flow nasal oxygen in critical care patients: a prospective pilot study. Intensive Care Med 37:1780–1786. https://doi.org/10.1007/s00134-011-2354-6
Takeishi N, Miki T, Otani T, Ii S, Morita K, Wada S (2019) Fluid dynamic assessment of tracheal flow in infants with congenital tracheal stenosis before and after surgery. Med Biol Eng Comput 57:837–847. https://doi.org/10.1007/s11517-018-1928-7
Thomas M, Joshi R, Cave G (2021) How much PEEP does high flow deliver via tracheostomy? a literature review and benchtop experiment. Crit Care Res Pract 2021:6036891. https://doi.org/10.1155/2021/6036891
Weibel ER, Gomez DM (1962) Architecture of the human lung. Science 137:577–585. https://doi.org/10.1126/science.137.3530.577
West JB, Luks AM (2021) West’s respiratory physiology. 11th edn. Wolters Kluwer, Philadelphia
Wilson TA (1967) Design of the bronchial tree. Nature 213:668–669. https://doi.org/10.1038/213668a0
Xiao Q, Cetto R, Doorly DJ, Bates AJ, Rose JN, McIntyre C, Comerford A, Madani G, Tolley NS, Schroter R (2020) Assessing changes in airflow and energy loss in a progressive tracheal compression before and after surgical correction. Ann Biomed Eng 48:822–833. https://doi.org/10.1007/s10439-019-02410-1
Yoshida T, Uchiyama A, Mashimo T, Fujino Y (2011) The effect of ventilator performance on airway pressure release ventilation: a model lung study. Anesth Analg 113:529–533. https://doi.org/10.1213/ANE.0b013e31821d72d0
Yoshida T, Torsani V, Gomes S, De Santis RR, Beraldo MA, Costa ELV, Tucci MR, Zin WA, Kavanagh BP, Amato MBP (2013) Spontaneous effort causes occult pendelluft during mechanical ventilation. Am J Respir Crit Care Med 188:1420–1427. https://doi.org/10.1164/rccm.201303-0539OC
Acknowledgements
This research was supported by JSPS KAKENHI Grant Numbers JP19H01175 and JP20H04504; by Osaka University Global Center for Medical Engineering and Informatics (MEI center); by the Keihanshin Consortium for Fostering the Next Generation of Global Leaders in Research (K-CONNEX), established by Human Resource Development Program for Science and Technology; and by MEXT as “Program for Promoting Researches on the Supercomputer Fugaku” (Development of personalized medical support technology based on simulation data science of whole brain blood circulation) (hp200136). The authors thank Drs. Naoto Yokoyama and Hiroshi Yamashita for their assistance with the preparation of this work.
Author information
Authors and Affiliations
Contributions
S.K. and N.T. analyzed data; H.T. and T.Y. performed experiments; S.K., N.T., and S.W. interpreted simulation results; N.T. prepared figures; N.T. drafted the manuscript; N.T. edited and revised the manuscript; S.K., N.T., H.T., T.Y., and S.W. approved the final version of the manuscript; N.T., T.Y., and S.W. contributed to the research conception and design. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kageyama, S., Takeishi, N., Taenaka, H. et al. Fluid dynamic assessment of positive end-expiratory pressure in a tracheostomy tube connector during respiration. Med Biol Eng Comput 60, 2981–2993 (2022). https://doi.org/10.1007/s11517-022-02649-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02649-2