Abstract
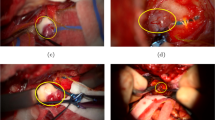
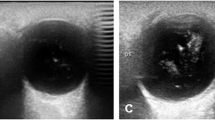
This paper presents an automated method for detection of the diagnostically prominent frames containing optic nerve sheath (ONS) from ocular ultrasonography video using deep learning; such frames are referred to as “Good View” frames in this paper. Vivid acquisition and measurement of diagnostic features during ultrasound imaging is a challenging task; it needs a highly skilled and experienced medical expert. Automated detection of the Good View frame and the subsequent automatic measurement of optic nerve sheath diameter (ONSD), predicting elevated intracranial pressure (ICP) status, will eliminate the need for frequent intervention of a medical expert for continuous monitoring and ICP status in traumatic patients. In the presented work, the proposed model automatically detects the appropriate frames containing ONS, from an ultrasound video, by using faster region-based CNN (Faster R-CNN) object detection model. The region proposal detection network finds the ONS by using bounding boxes. In addition, three CNN-based architectures are used for its feature extraction. Finally, SoftMax classifier classifies the ONS containing Good View frame. The Inceptionv2, ResNet50, and ResNet101 architectures are then compared by utilizing the optimized learning rate and epoch parameters for the CNN model so as to provide better detection of the Good View frame. The performance of the developed module has been analyzed by proposing a grading criterion of the Good View frame. Based on the detection score and mean opinion score, an USG frame is considered a Good View for a 95–99% detection score, and this Good View frame is used for measuring the ONSD value. It is found that Faster R-CNN ResNet101 (model 3) is an optimal model in terms of sensitivity and specificity for Good View frame detection at a learning rate of 0.0003. The sensitivity and specificity of this model are obtained as 90.41 and 91.45, respectively. Furthermore, the ONSD value is measured from Good View-detected frames using an automated algorithm involving image processing and computational methods. Considering the Good View frame (detection score 95–99), the algorithm-generated ONSD values are compared with the radiologist’s measured value of ONSD to validate the findings; a small percent root mean square difference (PRD) of 0.501 is found between these values, which is strong indicative of the accuracy of algorithm generated ONSD measurement using automatically detected Good View ocular USG frames.
Graphical Abstract


















Similar content being viewed by others
Data availability
The data used to support the findings of this study are included within the article.
References
Evensen KB, Eide PK (2020) Measuring intracranial pressure by invasive, less invasive or non-invasive means: limitations and avenues for improvement. Fluids Barriers CNS 17(1):1–33
Podkovik S, Kashyap S, Wiginton J IV, Kang C, Mo K, Goodrich M, Wolberg A, Wacker MR, Miulli DE (2020) Comparison of ventricular and lumbar cerebrospinal fluid composition. Cureus 12(7):e9315. https://doi.org/10.7759/cureus.9315
Bäuerle J, Schuchardt F, Schroeder L, Egger K, Weigel M, Harloff A (2013) Reproducibility and accuracy of optic nerve sheath diameter assessment using ultrasound compared to magnetic resonance imaging. BMC Neurol 13(1):1–6
Robba C, Santori G, Czosnyka M, Corradi F, Bragazzi N, Padayachy L, Taccone FS, Citerio G (2018) ONS diameter measured sonographically as non-invasive estimator of intracranial pressure: a systematic review and meta-analysis. Intensive Care Med 44(8):1284–1294
Lin J-J, Chen AE, Lin EE, Hsia S-H, Chiang M-C, Lin K-L (2020) Point-of-care ultrasound of ONS diameter to detect intracranial pressure in neurocritically ill children-a narrative review. Biomed J 43(3):231–239
Newman WD, Hollman AS, Dutton GN, Carachi R (2002) Measurement of ONS diameter by ultrasound: a means of detecting acute raised intracranial pressure in hydrocephalus. Br J Ophthalmol 86(10):1109–1113
Raghunandan N, Joseph M, Nithyanandam S, Karat S (2019) Role of ultrasonographic ONS diameter in the diagnosis and follow-up of papilledema and its correlation with Frisén’s severity grading. Indian J Ophthalmol 67(8):1310
Lahham S, Shniter I, Thompson M, Le D, Chadha T, Mailhot T, Lee Kang T, Chiem A, Tseeng S, Fox JC (2019) Point-of-care ultrasonography in the diagnosis of retinal detachment, vitreous hemorrhage, and vitreous detachment in the emergency department. JAMA Netw Open 2(4):e192162–e192162
Ballantyne SA, O’Neill G, Hamilton R, Hollman AS (2002) Observer variation in the sonographic measurement of ONS diameter in normal adults. Eur J Ultrasound 15:145–149
Kimberly HH, Shah S, Marill K, Noble V (2008) Correlation of ONS diameter with direct measurement of intracranial pressure. Acad Emerg Med 15(2):201–204
Tayal VS, Neulander M, Norton HJ, Foster T, Saunders T, Blaivas M (2007) Emergency department Sonographic measurement of ONS diameter to detect findings of increased intracranial pressure in adult head injury patients. Ann Emerg Med 49:508–514
Hansen HC, Helmke K, Kunze K (1994) ONS enlargement in acute intracranial hypertension. Neuro-Ophthalmology 14(6):345–354
Nag DS, Sahu S, Swain A, Kant S (2019) Intracranial pressure monitoring: Gold standard and recent innovations. World J Clin Cases 7(13):1535
Raboel PH, Bartek J, Andresen M, Bellander BM, Romner B (2012) Intracranial pressure monitoring: invasive versus non-invasive methods—a review. Crit Care Res Pract 2012 Article ID 950393, 1–14. https://doi.org/10.1155/2012/950393
Hassen GW, Bruck I, Donahue J, Mason B, Sweeney B, Saab W, Weedon J et al (2015) Accuracy of ONS diameter measurement by emergency physicians using bedside ultrasound. J Emerg Med 48(4):450–457
Liu D, Li Z, Zhang X, Zhao L, Jia J, Sun F, Wang Y, Ma D, Wei W (2017) Assessment of intracranial pressure with ultrasonographic retrobulbar optic nerve sheath diameter measurement. BMC Neurol 17(1):1–7
De La Hoz Polo M, Lluís AT, Segura OP, Bosque AA, Appiani CE, Mitjana JMC (2016) Ocular ultrasonography focused on the posterior eye segment: what radiologists should know. Insights Imaging 7(3):351–364
Patil P, Dasgupta B (2012) Role of diagnostic ultrasound in the assessment of musculoskeletal diseases. Ther Adv Musculoskelet Dis 4(5):341–355
Van der Gijp A, Van der Schaaf MF, Van der Schaaf IC, Huige JCBM, Ravesloot CJ, Van Schaik JPJ, ten Cate THJ (2014) Interpretation of radiological images: towards a framework of knowledge and skills. Adv Health Sci Educ 19(4):565–580
Gupta V, Gupta R, Kumar B, Pathak S, Saini R, Agrawal D (2019) A method for automated measurement of optic nerve sheath diameter from eye ultrasound image (IN Patent, 201811018251)
Girshick R, Donahue J, Darrell T, Malik J (2014) Rich feature hierarchies for accurate object detection and semantic segmentation. In Proceedings of the IEEE conference on computer vision and pattern recognition, pp 580–587
Girshick R (2015) Fast r-cnn. In Proceedings of the IEEE international conference on computer vision, pp 1440–1448
Ren S, He K, Girshick R, Sun J (2017) Faster R-CNN: towards real-time object detection with region proposal networks. IEEE Trans Patt Anal Mach Intell 39(6):1137–1149. https://doi.org/10.1109/TPAMI.2016.2577031
Szegedy C, Vanhoucke V, Ioffe S, Shlens J, Wojna Z (2013) Rethinking the inception architecture for computer vision. In Proceedings of the IEEE conference on computer vision and pattern recognition, pp 2818–2826
He K, Zhang X, Ren S, Sun J (2016) Deep residual learning for image recognition. In Proceedings of the IEEE conference on computer vision and pattern recognition, pp 770–778
Russakovsky O, Deng J, Hao Su, Krause J, Satheesh S, Ma S, Huang Z et al (2015) ImageNet large scale visual recognition challenge. Int J Comput Vision 115(3):211–252. https://doi.org/10.1007/s11263-015-0816-y
Lin T-Y, Maire M, Belongie S, Bourdev L, Girshick R, Hays J, Perona P, Ramanan D, Zitnick CL, Dollár P (2014) Microsoft COCO: common objects in context 2014 Sep 6, pp 740–755. http://arxiv.org/abs/1405.0312
Everingham M, Van Gool L, Williams CKI, Winn J, Zisserman A (2010) The pascal visual object classes (VOC) challenge. Int J Comput Vision 88(2):303–338. https://doi.org/10.1007/s11263-009-0275-4
Kuznetsova A, Rom H, Alldrin N, Uijlings J, Krasin I, Pont-Tuset J, Kamali S et al (2018) The open images dataset V4: unified image classification, object detection, and visual relationship detection at scale. CoRR ArXiv preprint. arXiv preprint arXiv:1811.00982
Author information
Authors and Affiliations
Contributions
All authors contributed equally in this work. All authors have read and approved the final manuscript and given their consent for publication of the article.
Corresponding author
Ethics declarations
Ethics approval
This article contains studies with human participants. No animals’ studies were involved in this review.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Singh, M., Kumar, B. & Agrawal, D. Good view frames from ultrasonography (USG) video containing ONS diameter using state-of-the-art deep learning architectures. Med Biol Eng Comput 60, 3397–3417 (2022). https://doi.org/10.1007/s11517-022-02680-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02680-3