Abstract
The recovery of independent gait represents one of the main functional goals of the rehabilitative interventions after stroke but it can be hindered by the presence of unilateral spatial neglect (USN). The aim of the paper is to study if the presence of USN in stroke patients affects lower limb gait parameters between the two body sides, differently from what could be expected by the motor impairment alone, and to explore whether USN is associated to specific gait asymmetry. Thirty-five stroke patients (right or left lesion and ischemic or hemorrhagic etiology) who regained independent gait were assessed for global cognitive functioning and USN. All patients underwent a gait analysis session by using a wearable inertial system, kinematic parameters were computed. Enrolled patients presented altered motion parameters. Stroke patients with USN showed specific asymmetries in the following parameters: stance phase, swing phase, and knee range of motion. No differences in the clinical scores were found as the presence of USN. The presence of USN was associated with a specific form of altered gait symmetry. These findings may help clinicians to develop more tailored rehabilitative training to enhance gait efficacy of patients with motor defects complicated by the presence of selected cognitive impairments.
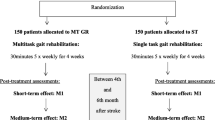
Graphical Abstract
Overview of the experiment setup. The workflow shows: diagnosis of unilateral spatial neglect by the neuropsychologist, sensors placement, gait analysis protocol and evaluation of the gait asymmetry together with the statistically significant features






Similar content being viewed by others
Data availability
The datasets generated during and/or analyzed during the current study are not publicly available due to privacy policy but are available from the corresponding author on a reasonable request.
Code availability
Not applicable.
References
Zamparo P, Francescato MP, De Luca G, Lovati L, di Prampera PE (1995) The energy cost of level walking in patients with hemiplegia. Scand J Med Sci Sports 5(6):348–352. https://doi.org/10.1111/j.1600-0838.1995.tb00057.x
Olney SJ, Richards C (1996) Hemiparetic gait following stroke. Part I: Characteristics Gait Posture 4(2):136–148. https://doi.org/10.1016/0966-6362(96)01063-6
Kimura Y, Yamada M, Ishiyama D, Nishio N, Kunieda Y, Koyama S, Sato A, Otobe Y, Ohji S, Suzuki M, Ogawa H, Ito D, Ichikawa T, Hamanaka K, Tanaka N, Muroh Y (2019) Impact of unilateral spatial neglect with or without other cognitive impairments on independent gait recovery in stroke survivors. J Rehabil Med 51(1):26–31. https://doi.org/10.2340/16501977-2503
Spaccavento S, Cellamare F, Falcone R, Loverre A, Nardulli R (2017) Effect of subtypes of neglect on functional outcome in stroke patients. Ann Phys Rehabil Med 60(6):376–381. https://doi.org/10.1016/j.rehab.2017.07.245
Morone G, Matamala-Gomez M, Sanchez-Vives MV, Paolucci S, Iosa M (2018) Watch your step! Who can recover stair climbing independence after stroke? Eur J Phys Rehabil Med 54(6):811–818. https://doi.org/10.23736/s1973-9087.18.04809-8
Alexander LD, Black SE, Patterson KK, Gao F, Danells CJ, McIlroy WE (2009) Association between gait asymmetry and brain lesion location in stroke patients. Stroke 40(2):537–544. https://doi.org/10.1161/STROKEAHA.108.527374
Kollen B, Van De Port I, Lindeman E, Twisk J, Kwakkel G (2005) Predicting improvement in gait after stroke: a longitudinal prospective study. Stroke 36(12):2676–2680. https://doi.org/10.1161/01.STR.0000190839.29234.50
Heilman KM, Bowers D, Valenstein E, Watson RT (1993) Disorders of visual attention. Baillière Clin Neurol 2(2):389–413
Pedersen PM, Jørgensen HS, Nakayama H, Raaschou HO, Olsen TS (1997) Hemineglect in acute stroke-incidence and prognostic implications: the Copenhagen stroke study1. Am J Phys Med Rehabil 76(2):122–127
Buxbaum LJ, Ferraro MK, Veramonti T, Farne A, Whyte JMDP, Ladavas E, Frassinetti F, Coslett HB (2004) Hemispatial neglect: subtypes, neuroanatomy, and disability. Neurology 62(5):749–756. https://doi.org/10.1212/01.WNL.0000113730.73031.F4
Laplane D, Degos JD (1983) Motor neglect. J Neurol Neurosurg Psychiatry 46(2):152–158. https://doi.org/10.1136/jnnp.46.2.152
Sapir A, Kaplan JB, He BJ, Corbetta M (2007) Anatomical correlates of directional hypokinesia in patients with hemispatial neglect. J Neurosci 27(15):4045–4051. https://doi.org/10.1523/JNEUROSCI.0041-07.2007
Katz N, Hartman-Maeir A, Ring H, Soroker N (1999) Functional disability and rehabilitation outcome in right hemisphere damaged patients with and without unilateral spatial neglect. Arch Phys Med Rehabil 80(4):379–384. https://doi.org/10.1016/S0003-9993(99)90273-3
Appelros P, Karlsson GM, Seiger Å, Nydevik I (2002) Neglect and anosognosia after first-ever stroke: incidence and relationship to disability. J Rehabil Med 34(5):215–220. https://doi.org/10.1080/165019702760279206
Lennon S, Ashburn A, Baxter D (2006) Gait outcome following outpatient physiotherapy based on the Bobath concept in people post stroke. Disabil Rehabil 28(13–14):873–881. https://doi.org/10.1080/09638280500535132
Grossi D, Lepore M, Napolitano A, Trojano L (2001) On selective left neglect during walking in a child. Brain Cogn 47(3):539–544. https://doi.org/10.1006/brcg.2001.1460
Vanbellingen T, Ottiger B, Maaijwee N, Pflugshaupt T, Bohlhalter S, Müri RM, Nef T, Cazzoli D, Nyffeler T (2017) Spatial neglect predicts upper limb use in the activities of daily living. Cerebrovasc Dis 44(3–4):122–127. https://doi.org/10.1159/000477500
Huitema RB, Brouwer WH, Hof AL, Dekker R, Mulder T, Postema K (2006) Walking trajectory in neglect patients. Gait Posture 23(2):200–205. https://doi.org/10.1016/j.gaitpost.2005.02.003
Pérennou D (2006) Postural disorders and spatial neglect in stroke patients: a strong association. Restor Neurol Neurosci 24(4–6):319–334
Chen P, Hreha K, Kong Y, Barrett AM (2015) Impact of spatial neglect on stroke rehabilitation: evidence from the setting of an inpatient rehabilitation facility. Arch Phys Med Rehabil 96(8):1458–1466. https://doi.org/10.1016/j.apmr.2015.03.019
Ferreira MS, Chamlian TR, França CN, Massaro AR (2015) Non-motor factors associated with the attainment of community ambulation after stroke. Clin Med Res 13(2):58–64. https://doi.org/10.3121/cmr.2014.1232
Duncan PW, Goldstein LB, Horner RD, Landsman PB, Samsa GP, Matchar DB (1994) Similar motor recovery of upper and lower extremities after stroke. Stroke 25(6):1181–1188. https://doi.org/10.1161/01.STR.25.6.1181
Goldie PA, Matyas TA, Kinsella GJ, Galea MP, Evans OM, Bach TM (1999) Prediction of gait velocity in ambulatory stroke patients during rehabilitation. Arch Phys Med Rehabil 80(4):415–420. https://doi.org/10.1016/S0003-9993(99)90278-2
Tromp E, Dinkla A, Mulder T (1995) Walking through doorways: an analysis of navigation skills in patients with neglect. Neuropsychol Rehabil 5(4):319–331. https://doi.org/10.1080/09602019508401475
Siciliano M, Chiorri C, Passaniti C, Sant’Elia V, Trojano L, Santangelo G (2020) Comparison of alternate and original forms of the Montreal Cognitive Assessment (MoCA): an Italian normative study. Neurol Sci 40(4):691–702. https://doi.org/10.1007/s10072-019-3700-7
Diller L, Weinberg J, Piasetsky E, Ruckdeschel-Hibbard M, Egelko S, Scotzin M, Gordon W (1974) Methods for the evaluation and treatment of the visual perceptual difficulties of right brain damaged individuals. New York University Medical Center. In Suppl 8th Annu Work Rehabil Prof
Mahoney FI, Barthel DW (1965) Functional evaluation: the Barthel Index: a simple index of independence useful in scoring improvement in the rehabilitation of the chronically ill. Md State Med J 14:61–65
Donisi L, Pagano G, Cesarelli G, Coccia A, Amitrano F, D’Addio G (2021) Benchmarking between two wearable inertial systems for gait analysis based on a different sensor placement using several statistical approaches. Measurement 173:108642 https://doi.org/10.1016/j.measurement.2020.108642
Mancini M, Horak FB (2016) Potential of APDM mobility lab for the monitoring of the progression of Parkinson’s disease. Expert Rev Med Devices 13(5):455–462. https://doi.org/10.1586/17434440.2016.1153421
Morris R, Stuart S, McBarron G, Fino PC, Mancini M, Curtze C (2019) Validity of mobility lab (version 2) for gait assessment in young adults, older adults and Parkinson’s disease. Physiol Meas 40(9):095003. https://doi.org/10.1088/1361-6579/ab4023
Schmitz-Hübsch T, Brandt AU, Pfueller C, Zange L, Seidel A, Kühn AA, Paul F, Minnerop M, Doss S (2016) Accuracy and repeatability of two methods of gait analysis–GaitRite™ und mobility lab™–in subjects with cerebellar ataxia. Gait Posture 48:194–201. https://doi.org/10.1016/j.gaitpost.2016.05.014
Mancini M, King L, Salarian A, Holmstrom L, McNames J, Horak FB (2011) Mobility lab to assess balance and gait with synchronized body-worn sensors. J Bioeng Biomed Sci 007 https://doi.org/10.4172/2155-9538.S1-007
D’Addio G, Donisi L, Pagano G, Improta G, Biancardi A, Cesarelli M (2019) Agreement between Opal and G-walk wearable inertial systems in gait analysis on normal and pathological subjects. Proceedings of the 2019 41st Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC), Berlin, Germany, July 23–27 2019; Barbieri, R., Eds.; IEEE: Piscataway, USA, 3286–3289 https://doi.org/10.1109/EMBC.2019.8857841
Pagano G, D’Addio G, De Campi M, Donisi L, Biancardi A, Cesarelli M (2020) Rehabilitation outcome in patients undergone hip or knee replacement surgery using inertial technology for gait analysis. Proceedings of the 2020 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, June-July 1–1 2020; IEEE: Piscataway, USA, 5 https://doi.org/10.1109/MeMeA49120.2020.9137125
Coccia A, Lanzillo B, Donisi L, Amitrano F, Cesarelli G, D’Addio G (2020) Repeatability of spatio-temporal gait measurements in Parkinson’s disease. Proceedings of the 2020 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, June-July 1–1 2020; IEEE: Piscataway, USA, 5 https://doi.org/10.1109/MeMeA49120.2020.9137357
Normative Data Used in Mobility Lab v2. Available online: normative data used in mobility lab v2 – product support and information (apdm.com) (accessed on 9 April 2021).
Wonsetler EC, Bowden MG (2017) A systematic review of mechanisms of gait speed change post-stroke. Part 1: spatiotemporal parameters and asymmetry ratios. Topics Stroke Rehabil 24(6):435–446. https://doi.org/10.1080/10749357.2017.1285746
Sibley KM, Tang A, Brooks D, McIlroy WE (2008) Effects of extended effortful activity on spatio-temporal parameters of gait in individuals with stroke. Gait Posture 27(3):387–392. https://doi.org/10.1016/j.gaitpost.2007.05.007
Yang S, Zhang JT, Novak AC, Brouwer B, Li Q (2013) Estimation of spatio-temporal parameters for post-stroke hemiparetic gait using inertial sensors. Gait Posture 37(3):354–358. https://doi.org/10.1016/j.gaitpost.2012.07.032
Patterson KK, Parafianowicz I, Danells CJ, Closson V, Verrier MC, Staines WR, Black SE, McIlroy WE (2008) Gait asymmetry in community-ambulating stroke survivors. Arch Phys Med Rehabil 89(2):304–310. https://doi.org/10.1016/j.apmr.2007.08.142
Author information
Authors and Affiliations
Contributions
Conceptualization, Pasquale Moretta, Leandro Donisi, and Giovanni D’Addio; methodology, Pasquale Moretta and Leandro Donisi; software, Leandro Donisi; validation, Pietro Balbi and Luigi Trojano; formal analysis, Pasquale Moretta and Leandro Donisi; investigation, Pasquale Moretta, Leandro Donisi and Giovanni D’Addio; resources, Pietro Balbi and Giovanni D’Addio; data curation, Pasquale Moretta, Leandro Donisi and Giuseppe Cesarelli; writing—original draft preparation, Pasquale Moretta and Leandro Donisi.; writing—review and editing, Pietro Balbi, Luigi Trojano and Giovanni D’Addio; visualization, Pasquale Moretta, Leandro Donisi and Giuseppe Cesarelli; supervision, Pietro Balbi, Luigi Trojani and Giovanni D’Addio; project administration, Pietro Balbi and Giovanni D’Addio.
Corresponding author
Ethics declarations
Ethics approval
The study was conducted according to the guidelines of the Declaration of Helsinki.
Consent to participate
Informed consent was obtained from all subjects involved in the study.
Consent for publication
Informed consent was obtained from all subjects involved in the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Moretta, P., Donisi, L., Balbi, P. et al. Gait asymmetry in stroke patients with unilateral spatial neglect. Med Biol Eng Comput 61, 651–659 (2023). https://doi.org/10.1007/s11517-022-02738-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02738-2