Abstract
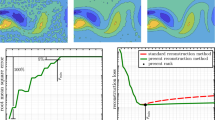
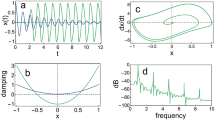
This work studied, for the first time, the time–frequency characteristics of the vibrations underlying the first fetal heart sound (S1). To this end, the continuous wavelet transform was used to produce time-energy and time–frequency representations of S1 from where five vibrations were studied by their timing, energy, and frequency characteristics in three gestational age groups (early, G1, preterm, G2, and term, G3). Results on a dataset of 1111 S1s (9 phonocardiograms between 33 and 40 weeks) indicate that such representations uncovered a set of five well-defined, non-overlapped, and large-energy vibrations whose features presented interesting behaviors. Thus, for each group, while the timing characteristics of the five vibrations were likely to be statically different, their frequencies were similar. Also, the energies of the vibrations were likely to be different only in G2 and G3. Alternatively, while the frequencies and energies of each vibration were likely to statistically change among groups (excluding the energy of the third vibration), the timings were more likely to change only from G1 to G2 and from G2 to G3. Therefore, this methodology seems suitable to detect and study the generating vibrations of S1. Future work will test the correlation between these vibrations and the valvular events.
Graphical Abstract









Similar content being viewed by others
References
Nagel J (1986) New diagnostic and technical aspects of fetal phonocardiography. Eur J Obstet Gynecol Reprod Biol 23(5–6):295–303. https://doi.org/10.1016/0028-2243(86)90163-2
Adithya PC, Sankar R, Moreno WA, Hart S (2017) Trends in fetal monitoring through phonocardiography: challenges and future directions. Biomed Signal Process Control 33:289–305. https://doi.org/10.1016/j.bspc.2016.11.007
Kovács F, Horváth C, Balogh AT, Hosszú G (2011) Fetal phonocardiography–past and future possibilities. Comput Methods Programs Biomed 104(1):19–25. https://doi.org/10.1016/j.cmpb.2010.10.006
Bhoi AK, Sherpa KS, Khandelwal B (2015) Multidimensional analytical study of heart sounds: a review. Int J Bioautomation 19(3):351–376
Chourasia J, Chourasia VS, Mittra AK (2017) Prenatal identification of CHD murmur using four segment phonocardiographic signal analysis. J Med Eng Technol 41(2):122–130. https://doi.org/10.1080/03091902.2016.1239277
Várady P, Wildt L, Benyó Z, Hein A (2003) An advanced method in fetal phonocardiography. Comput Methods Programs Biomed 71(3):283–296. https://doi.org/10.1016/S0169-2607(02)00111-6
Moghavvemi M (2003) A non-invasive PC-based measurement of fetal phonocardiography. Sens Actuators, A 107(1):96–103. https://doi.org/10.1016/S0924-4247(03)00254-1
Talbert DG, Davies WL, Johnson F, Abraham N, Colley N, Southall DP (1986) Wide bandwidth fetal phonography using a sensor matched to the compliance of the mother’s abdominal wall. Biomed Eng, IEEE Trans BME33(2):175–181. https://doi.org/10.1109/TBME.1986.325850
Bassil HE, Dripps JH (1989) Real time processing and analysis of fetal phonocardiographic signals. Clin Phys Physiol Meas 10(4B):67–74. https://doi.org/10.1088/0143-0815/10/4B/011
Chourasia VS, Mittra AK (2012) Passive acoustic signal acquisition system for non-invasive fetal heart sound monitoring applications. Internet J Med Technol 5(1):1–8. https://doi.org/10.5580/55f
Zuckerwar AJ, Pretlow RA, Stoughton JW, Baker DA (1993) Development of a piezopolymer pressure sensor for a portable fetal heart rate monitor. Biomed Eng, IEEE Trans 40(9):963–969. https://doi.org/10.1109/10.245618
Jiménez-González A, James CJ (2009) Extracting sources from noisy abdominal phonograms: a single-channel blind source separation method. Med Biol Eng Compu 47(6):655–664. https://doi.org/10.1007/s11517-009-0474-8
Jiménez-González A, James CJ (2013) Blind separation of multiple physiological sources from a single-channel recording: a preprocessing approach for antenatal surveillance. IX Int Seminar Med Inform Process Anal 8922:89220D. https://doi.org/10.1117/12.2035520
Chourasia VS, Tiwari AK, Gangopadhyay R (2014) A novel approach for phonocardiographic signals processing to make possible fetal heart rate evaluations. Digit Signal Process 30:165–183. https://doi.org/10.1016/j.dsp.2014.03.009
Martinek R et al (2020) Passive fetal monitoring by advanced signal processing methods in fetal phonocardiography. IEEE Access 8:221942. https://doi.org/10.1109/ACCESS.2020.3043496
Tomassini S et al (2019) Wavelet filtering of fetal phonocardiography: a comparative analysis. Math Biosci Eng 16(5):6034–6046. https://doi.org/10.3934/mbe.2019302
Koutsiana E, Hadjileontiadis LJ, Chouvarda I, Khandoker AH (2017) Fetal heart sounds detection using wavelet transform and fractal dimension. Front Bioeng Biotechnol 5:1–9. https://doi.org/10.3389/fbioe.2017.00049
Jiménez-González A, James CJ (2013) Antenatal surveillance through estimates of the sources underlying the abdominal phonogram: a preliminary study. Physiol Meas 34(9):1041–1061. https://doi.org/10.1088/0967-3334/34/9/1041
Fleming JEE, Raymond SPW, Smith GCS, Whitfield CR (1986) The measurement of fetal systolic time intervals: lessons from ultrasound. Eur J Obstet Gynecol Reprod Biol 23(5–6):289–294. https://doi.org/10.1016/0028-2243(86)90162-0
Mittra AK, Choudhari NK (2009) Development of a low cost fetal heart sound monitoring system for home care application. J Biomed Sci Eng 02(06):380–389. https://doi.org/10.4236/jbise.2009.26055
Jiménez-González A, James CJ (2012) On the interpretation of the independent components underlying the abdominal phonogram: a study of their physiological relevance. Physiol Meas 33(2):297–314. https://doi.org/10.1088/0967-3334/33/2/297
Baskaran A, Sivalingam N (1996) Fetal heart sound analysis: a preliminary evaluation. Med J Malaysia 51(1):64–67
Zahorian SA, Zuckerwar AJ, Karnjanadecha M (2012) Dual transmission model and related spectral content of the fetal heart sounds. Comput Methods Programs Biomed 108(1):20–27. https://doi.org/10.1016/j.cmpb.2011.12.006
Kovács F, Horváth C, Balogh AT, Hosszú G (2011) Extended noninvasive fetal monitoring by detailed analysis of data measured with phonocardiography. IEEE Trans Biomed Eng 58(1):64–70. https://doi.org/10.1109/TBME.2010.2071871
Kovács F et al (2015) Screening of congenital heart diseases with fetal phonocardiography. Int J Med Health Biomed Bioeng Pharm Eng 9(6):436–440
Mittra AK, Choudhari NK (2009) Spectral estimation techniques for advanced fetal phono cardiography. i managers J Fut Eng Technol 4(3):30–36. https://doi.org/10.26634/jfet.4.3.277
Chourasia VS, Mittra AK (2009) A comparative analysis of de-noising algorithms for fetal phonocardiographic signals. IETE J Res 55(1):10–15. https://doi.org/10.4103/0377-2063.51322
Chourasia VS, Tiwari AK, Gangopadhyay R (2011) Time-frequency characterization of fetal phonocardiographic signals using wavelet scalogram. J Mech Med Biol 11(2):391–406. https://doi.org/10.1142/S0219519410003782
Reinhold J, Rudhe U (1957) Relation of the first and second heart sounds to events in the cardiac cycle. Br Heart J 19(4):473–485. https://doi.org/10.1136/hrt.19.4.473
Laniado S, Yellin EL, Miller H, Frater RW (1973) Temporal relation of the first heart sound to closure of the mitral valve. Circulation 47(5):1006–1014. https://doi.org/10.1161/01.CIR.47.5.1006
Ergen B, Tatar Y, Gulcur HO (2012) Time-frequency analysis of phonocardiogram signals using wavelet transform: a comparative study. Comput Methods Biomech Biomed Engin 15(4):371–381. https://doi.org/10.1080/10255842.2010.538386
Djebbari A, Bereksi-Reguig F (2011) A new chirp – based wavelet for heart sounds time – frequency analysis. Int J Commun Antenna Propag 1(1):92–102. https://doi.org/10.1186/1475-925X-12-37
Khandoker AH, Kimura Y, Ito T, Sato N, Okamura K, Palaniswami M (2009) Antepartum non-invasive evaluation of opening and closing timings of the cardiac valves in fetal cardiac cycle. Med Biol Eng Compu 47(10):1075–1082. https://doi.org/10.1007/s11517-009-0528-y
Purisch SE, Gyamfi-Bannerman C (2017) Epidemiology of preterm birth. Semin Perinatol 41(7):387–391. https://doi.org/10.1053/j.semperi.2017.07.009
Debbal S (2007) Graphic representation and analysis of the PCG signal using the continuous wavelet transform. Internet J Bioeng 2(2):1–7. https://doi.org/10.5580/1ab4
Armstrong RA (2014) When to use the Bonferroni correction. Ophthalmic Physiol Opt 34:502–508. https://doi.org/10.1111/opo.12131
Murata Y, Martin C (1974) Systolic time intervals of the fetal cardiac cycle. Clin Obstet Gynaecol 44(2):224–232. https://doi.org/10.1016/S0950-3552(87)80029-9
Marzbanrad F et al (2014) Automated estimation of fetal cardiac timing events from doppler ultrasound signal using hybrid models. IEEE J Biomed Health Inform 18(4):1169–1177. https://doi.org/10.1109/JBHI.2013.2286155
Alnuaimi S, Jimaa S, Kimura Y, Apostolidis GK, Hadjileontiadis LJ, Khandoker AH (2019) Fetal cardiac timing events estimation from doppler ultrasound signals using swarm decomposition. Front Physiol 10:1–13. https://doi.org/10.3389/fphys.2019.00789
Mensah-Brown NA, Wakai RT, Cheulkar B, Srinivasan S, Strasburger JF (2010) Assessment of left ventricular pre-ejection period in the fetus using simultaneous magnetocardiography and echocardiography. Fetal Diagn Ther 28(3):167–174. https://doi.org/10.1159/000318345
Cesarelli M, Ruffo M, Romano M, Bifulco P (2012) Simulation of foetal phonocardiographic recordings for testing of FHR extraction algorithms. Comput Methods Programs Biomed 107(3):513–523. https://doi.org/10.1016/j.cmpb.2011.11.008
ChetlurAdithya P, Sankar R, Moreno WA, Hart S (2017) Trends in fetal monitoring through phonocardiography: challenges and future directions. Biomed Sig Process Control 33:289–305. https://doi.org/10.1016/j.bspc.2016.11.007
Acknowledgements
Usiel Salas-Márquez thanks CONACyT for sponsoring his MsC studies.
Author information
Authors and Affiliations
Contributions
Aída Jiménez-González: conceptualization, investigation, supervision, and writing (original draft and the revised versions); Usiel Salas-Márquez: methodology, formal, and statistical analysis.
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Jiménez-González, A., Salas-Márquez, U. Time–frequency characteristics of the vibrations underlying the first fetal heart sound: a preliminary study. Med Biol Eng Comput 61, 739–756 (2023). https://doi.org/10.1007/s11517-022-02756-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-022-02756-0