Abstract
The midpalatal suture (MPS) corresponds to the tissue that joins the two maxillary bones. Understanding the mechanical behavior of this tissue is of particular interest to those patients who require orthodontic treatments such as Rapid Maxillary Expansion (RME). The objective of this research was to observe the influence of interdigitation and collagen fibers on the mechanical response of MPS. To this end, a finite element analysis in two-dimensional models of the bone-suture-bone interface was performed considering the characteristics of the MPS. The geometry of the suture was modeled with 4 different levels of interdigitation: null, moderate, scalloped and fractal. The influence of collagen fibers, aligned transversely along the suture, was considered by incorporating linked structures of the bone fronts. According to the results, the factor that has the greatest impact on the magnitude and distribution of stresses is the interdigitation degree. A higher level of interdigitation produces an increase in tissue stiffness and a lower influence of collagen fibers on the mechanical response of the tissue. Therefore, this research contributes to the understanding of the MPS biomechanics by providing information that may be useful to health staff when evaluating the feasibility of procedures such as RME.
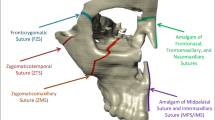
Graphical Abstract









Similar content being viewed by others
Data availability
Not applicable.
References
Beederman M, Farina EM, Reid RR (2014) Molecular basis of cranial suture biology and disease: Osteoblastic and osteoclastic perspectives. Genes Dis 1(1):120–125. https://doi.org/10.1016/j.gendis.2014.07.004
Maloul A, Fialkov J, Wagner D, Whyne CM (2014) Characterization of craniofacial sutures using the finite element method. J Biomech 47(1):245–252. https://doi.org/10.1016/j.jbiomech.2013.09.009
Khonsari RH et al (2013) A mathematical model for mechanotransduction at the early steps of suture formation. Proc R Soc B Biol Sci 280(1759):20122670–20122670. https://doi.org/10.1098/rspb.2012.2670
Anderson D (2013) Mosby’s Pocket Dictionary of Medicine, Nursing & Health, 7th ed. Mosby Elsevier
Ennes J. P. and Consolaro A (2002) “Análise morfológica da sutura palatina mediana de ratos, de coelhos, de macacos e homens em diferentes fases do desenvolvimento cronológico,” Universidade de São Paulo
Angelieri F, Cevidanes LHS, Franchi L, Gonçalves JR, Benavides E, McNamara JA (2013) Midpalatal suture maturation: Classification method for individual assessment before rapid maxillary expansion. Am J Orthod Dentofac Orthop 144(5):759–769. https://doi.org/10.1016/j.ajodo.2013.04.022
Melsen B (1975) Palatal growth studied on human autopsy material. A histologic microradiographic study. Am J Orthod 68(1):42–54. https://doi.org/10.1016/0002-9416(75)90158-X
Thadani M, Shenoy U, Patle B, Kalra A, Goel S, Toshinawal N (2010) “Midpalatal Suture Ossification and Skeletal Maturation: A Comparative Computerized Tomographic Scan and Roentgenographic Study.” J Indian Acad Oral Med Radiol 22 (2)81–87 [Online]. Available: ------------
Suzuki H, Moon W, Previdente LH, Suzuki SS, Garcez AS, Consolaro A (2016) Miniscrew-assisted rapid palatal expander (MARPE): the quest for pure orthopedic movement. Dental Press J Orthod 21(4):17–23. https://doi.org/10.1590/2177-6709.21.4.017-023.oin
Ramieri GA, Spada MC, Austa M, Bianchi SD, Berrone S (2005) Transverse maxillary distraction with a bone-anchored appliance: Dento-periodontal effects and clinical and radiological results. Int J Oral Maxillofac Surg 34(4):357–363. https://doi.org/10.1016/j.ijom.2004.10.011
Garreau E, Bouscaillou J, Rattier S, Ferri J, Raoul G (2016) Bone-borne distractor versus tooth-borne distractor for orthodontic distraction after surgical maxillary expansion: The patient’s point of view. Int Orthod 14(2):214–232. https://doi.org/10.1016/j.ortho.2016.03.013
Lione R, Franchi L, Cozza P (2013) Does rapid maxillary expansion induce adverse effects in growing subjects? Angle Orthod 83(1):172–182. https://doi.org/10.2319/041012-300.1
Provatidis C, Georgiopoulos B, Kotinas A, McDonald JP (2007) On the FEM modeling of craniofacial changes during rapid maxillary expansion. Med Eng Phys 29(5):566–579. https://doi.org/10.1016/j.medengphy.2006.03.007
Kumar A, Gurunathan D, Muruganandham, Sharma S (2011) Rapid Maxillary Expansion : A Unique Treatment Modality in Dentistry. J Clin an Diagnostic Res 5(4):906–911
Hou B, Kolpakova-Hart E, Fukai N, Wu K, Olsen BR (2009) The polycystic kidney disease 1 (Pkd1) gene is required for the responses of osteochondroprogenitor cells to midpalatal suture expansion in mice. Bone 44(6):1121–1133. https://doi.org/10.1016/j.bone.2009.02.018
Liu SSY, Opperman LA, Kyung HM, Buschang PH (2011) Is there an optimal force level for sutural expansion? Am J Orthod Dentofac Orthop 139(4):446–455. https://doi.org/10.1016/j.ajodo.2009.03.056
Burn A, Herring S, Hubbard R, Zink K, Rafferty K, Lieberman D (2010) Dietary consistency and the midline sutures in growing pigs. Orthod Craniofac Res 13(2):106–113. https://doi.org/10.1111/j.1601-6343.2010.01483.x
Liu L et al (2017) The effects of morphological irregularity on the mechanical behavior of interdigitated biological sutures under tension. J Biomech 58:71–78. https://doi.org/10.1016/j.jbiomech.2017.04.017
Romanyk DL et al (2013) Towards a viscoelastic model for the unfused midpalatal suture: Development and validation using the midsagittal suture in New Zealand white Rabbits. J Biomech 46(10):1618–1625. https://doi.org/10.1016/j.jbiomech.2013.04.011
Zollikofer CPE, Weissmann JD (2011) A bidirectional interface growth model for cranial interosseous suture morphogenesis. J Anat 219(2):100–114. https://doi.org/10.1111/j.1469-7580.2011.01386.x
Hou B, Fukai N, Olsen BR (2007) Mechanical force-induced midpalatal suture remodeling in mice. Bone 40(6):1483–1493. https://doi.org/10.1016/j.bone.2007.01.019
Henderson JH, Chang LY, Song HM, Longaker MT, Carter DR (2005) Age-dependent properties and quasi-static strain in the rat sagittal suture. J Biomech 38(11):2294–2301. https://doi.org/10.1016/j.jbiomech.2004.07.037
Parr JA, Garetto LP, Wohlford ME, Arbuckle GR, Roberts WE (1997) Sutural expansion using rigidly integrated endosseous implants an experimental study in rabbits.pdf. Angle Orthod 67(4):283–290
Oppenheimer AJ, Rhee ST, Goldstein SA, Buchman SR (2012) Force-induced craniosynostosis via paracrine signaling in the murine sagittal suture. J Craniofac Surg 23(2):573–577. https://doi.org/10.1097/SCS.0b013e318241db3e
Peptan AI, Lopez A, Kopher RA, Mao JJ (2008) Responses of intramembranous bone and sutures upon in vivo cyclic tensile and compressive loading. Bone 42(2):432–438. https://doi.org/10.1016/j.bone.2007.05.014
Vij K, Mao JJ (2006) Geometry and cell density of rat craniofacial sutures during early postnatal development and upon in vivo cyclic loading. Bone 38(5):722–730. https://doi.org/10.1016/j.bone.2005.10.028
Hirukawa K, Miyazawa K, Maeda H, Kameyama Y, Goto S, Togari A (2005) Effect of tensile force on the expression of IGF-I and IGF-I receptor in the organ-cultured rat cranial suture. Arch Oral Biol 50(3):367–372. https://doi.org/10.1016/j.archoralbio.2004.07.003
Sawada M and Shimizu N (1996) “Stimulation of bone formation in the expanding mid-palatal suture by transforming growth factor-S , in the rat.” Eur J Orthod 18(2):169–179 [Online]. Available: http://www.scopus.com/inward/record.url?eid=2-s2.0-0030119188&partnerID=40&md5=c974b50686c4dc8eb7bb9b8195f70f8e.
Yoshimura K, Kobayashi R, Ohmura T, Kajimoto Y, Miura T (2016) A new mathematical model for pattern formation by cranial sutures. J Theor Biol 408:66–74. https://doi.org/10.1016/j.jtbi.2016.08.003
Burgos-Flórez FJ, Gavilán-Alfonso ME, Garzón-Alvarado DA (2016) Flat bones and sutures formation in the human cranial vault during prenatal development and infancy: A computational model. J Theor Biol 393:127–144. https://doi.org/10.1016/j.jtbi.2016.01.006
Miura T et al (2009) Mechanism of skull suture maintenance and interdigitation. J Anat 215(6):642–655. https://doi.org/10.1111/j.1469-7580.2009.01148.x
Jasinoski SC, Reddy BD, Louw KK, Chinsamy A (2010) Mechanics of cranial sutures using the finite element method. J Biomech 43(16):3104–3111. https://doi.org/10.1016/j.jbiomech.2010.08.007
Jasinoski SC, Reddy BD (2012) Mechanics of cranial sutures during simulated cyclic loading. J Biomech 45(11):2050–2054. https://doi.org/10.1016/j.jbiomech.2012.05.007
Korbmacher H, Schilling A, Püschel K, Amling M, Kahl-Nieke B (2007) Dreidimensionale mikro-computertomographische Analyse der humanen Sutura palatina mediana in Abhängigkeit vom Alter. J Orofac Orthop 68(5):364–376. https://doi.org/10.1007/s00056-007-0729-7
Ludwig B et al (2013) Application of a new viscoelastic finite element method model and analysis of miniscrew-supported hybrid hyrax treatment. Am J Orthod Dentofac Orthop 143(3):426–435. https://doi.org/10.1016/j.ajodo.2012.07.019
Franchi L, Baccetti T, Lione R, Fanucci E, Cozza P (2010) Modifications of midpalatal sutural density induced by rapid maxillary expansion: A low-dose computed-tomography evaluation. Am J Orthod Dentofac Orthop 137(4):486–488. https://doi.org/10.1016/j.ajodo.2009.10.028
Carvalho Trojan Serpe L, Barbosa de Las Casas E, Toyofuku Moreira Melo AC, González-Torres LA (2015)“A bilinear elastic constitutive model applied for midpalatal suture behavior during rapid maxillary expansion.” Rev Bras Eng Biomed 31 4 319–327 https://doi.org/10.1590/2446-4740.0637
Lee HK et al (2014) Stress distribution and displacement by different bone-borne palatal expanders with micro-implants: A three-dimensional finite-element analysis. Eur J Orthod 36(5):531–540. https://doi.org/10.1093/ejo/cjs063
de Sousa Araugio RM, Landre J Jr, de Lourdes Almeida Silva D, Pacheco W, Pithon MM, Oliveira DD (2013) Influence of the expansion screw height on tshe dental effects of the hyrax expander: A study with finite elements. Am J Orthod Dentofac Orthop 143(2):221–227. https://doi.org/10.1016/j.ajodo.2012.09.016
Lee H, Ting K, Nelson M, Sun N, Sung SJ (2009) Maxillary expansion in customized finite element method models. Am J Orthod Dentofac Orthop 136(3):367–374. https://doi.org/10.1016/j.ajodo.2008.08.023
Lodish H, Berk A, Zipursky SL, Matsudaira P, Baltimore D, Darnell J (2000) Molecular Cell Biology, 4th edn. W. H. Freeman, New York
Karimui RY (2021) “A new approach to measure the fractal dimension of a trajectory in the high-dimensional phase space.” Chaos, Solitons and Fractals 151 https://doi.org/10.1016/j.chaos.2021.111239
Chamorro-Posada P (2016) A simple method for estimating the fractal dimension from digital images: The compression dimension. Chaos, Solitons Fractals 91:562–572. https://doi.org/10.1016/j.chaos.2016.08.002
Yao K, Chen H, Peng WL, Wang Z, Yao J, Wu Y (2021) A new method on Box dimension of Weyl-Marchaud fractional derivative of Weierstrass function. Chaos, Solitons Fractals 142:1–5. https://doi.org/10.1016/j.chaos.2020.110317
Romanyk DL, Shim C, Liu SS, Lagravere MO, Major PW, Carey JP (2016) Viscoelastic response of the midpalatal suture during maxillary expansion treatment. Orthod Craniofacial Res 19(1):28–35. https://doi.org/10.1111/ocr.12106
Macginnis M, Chu H, Youssef G, Wu KW, Machado AW, Moon W (2014)“The effects of micro-implant assisted rapid palatal expansion (MARPE) on the nasomaxillary complex — a Finite Element Method (FEM) analysis.” Prog Orthod 1–15. https://doi.org/10.1186/s40510-014-0052-y
Romanyk DL, Collins CR, Lagravere MO, Toogood RW, Major PW, Carey JP (2013) Role of the midpalatal suture in FEA simulations of maxillary expansion treatment for adolescents: A review. Int Orthod 11(2):119–138. https://doi.org/10.1016/j.ortho.2013.02.001
Carvalho Trojan L, Andrés González-Torres L, Claudia Moreira Melo A, Barbosa de Las Casas E (2017) “Stresses and Strains Analysis Using Different Palatal Expander Appliances in Upper Jaw and Midpalatal Suture.” Artif Organs 41(6):E41–E51 https://doi.org/10.1111/aor.12817.
Del Santo M, Minarelli AM, Liberti EA (1998) Morphological aspects of the mid-palatal suture in the human foetus: A light and scanning electron microscopy study. Eur J Orthod 20(1):93–99. https://doi.org/10.1093/ejo/20.1.93
Acknowledgements
Not applicable
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. The implementation of the computational models and the obtaining of results were carried out by José Alejandro Guerrero Vargas. Analysis and discussion of the results were performed by all authors. The first draft of the manuscript was written by José Alejandro Guerrero Vargas and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
The author(s) consent to the publication of this article.
Competing interests
The author(s) declared no potential conflicts of interests with respect to the research, authorship, and publications of this paper.
Declarations of interest
None.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Guerrero Vargas, J.A., Carvalho Trojan, L., de Las Casas, E.B. et al. Finite element analysis of the influence of interdigitation pattern and collagen fibers on the mechanical behavior of the midpalatal suture. Med Biol Eng Comput 61, 2367–2377 (2023). https://doi.org/10.1007/s11517-023-02838-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-023-02838-7