Abstract
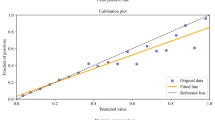
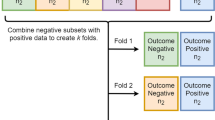
Revision total knee arthroplasty (TKA) is associated with a higher risk of readmission than primary TKA. Identifying individual patients predisposed to readmission can facilitate proactive optimization and increase care efficiency. This study developed machine learning (ML) models to predict unplanned readmission following revision TKA using a national-scale patient dataset. A total of 17,443 revision TKA cases (2013–2020) were acquired from the ACS NSQIP database. Four ML models (artificial neural networks, random forest, histogram-based gradient boosting, and k-nearest neighbor) were developed on relevant patient variables to predict readmission following revision TKA. The length of stay, operation time, body mass index (BMI), and laboratory test results were the strongest predictors of readmission. Histogram-based gradient boosting was the best performer in distinguishing readmission (AUC: 0.95) and estimating the readmission probability for individual patients (calibration slope: 1.13; calibration intercept: -0.00; Brier score: 0.064). All models produced higher net benefit than the default strategies of treating all or no patients, supporting the clinical utility of the models. ML demonstrated excellent performance for the prediction of readmission following revision TKA. Optimization of important predictors highlighted by our model may decrease preventable hospital readmission following surgery, thereby leading to reduced financial burden and improved patient satisfaction.
Graphical Abstract




Similar content being viewed by others
References
Papakostidis C, Giannoudis PV, Watson JT, Zura R, Steen RG (2021) Serious adverse events and 30-day hospital readmission rate following elective total knee arthroplasty: a systematic review and meta-analysis. J Orthop Surg Res 16:236. https://doi.org/10.1186/s13018-021-02358-w
Belmont PJ, Goodman GP, Rodriguez M, Bader JO, Waterman BR, Schoenfeld AJ (2016) Predictors of hospital readmission following revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 24:3329–3338. https://doi.org/10.1007/s00167-015-3782-6
Pugely AJ, Callaghan JJ, Martin CT, Cram P, Gao Y (2013) Incidence of and risk factors for 30-day readmission following elective primary total joint arthroplasty: analysis from the ACS-NSQIP. J Arthroplasty 28:1499–1504. https://doi.org/10.1016/j.arth.2013.06.032
Schairer WW, Vail TP, Bozic KJ (2014) What are the rates and causes of hospital readmission after total knee arthroplasty? Clin Orthop Relat Res 472:181–187. https://doi.org/10.1007/s11999-013-3030-7
Gould D, Dowsey MM, Spelman T, Jo O, Kabir W, Trieu J, Bailey J, Bunzli S, Choong P (2021) Patient-related risk factors for unplanned 30-day hospital readmission following primary and revision total knee arthroplasty: a systematic review and meta-analysis. J Clin Med 10:134. https://doi.org/10.3390/jcm10010134
Phillips JLH, Rondon AJ, Vannello C, Fillingham YA, Austin MS, Courtney PM (2019) How much does a readmission cost the bundle following primary hip and knee arthroplasty? J Arthroplasty 34:819–823. https://doi.org/10.1016/j.arth.2019.01.029
Phruetthiphat O, Otero JE, Zampogna B, Vasta S, Gao Y, Callaghan JJ (2020) Predictors for readmission following primary total hip and total knee arthroplasty. J Orthop Surg (Hong Kong) 28:230949902095916. https://doi.org/10.1177/2309499020959160
Courtney PM, Boniello AJ, Della Valle CJ, Lee G-C (2018) Risk adjustment is necessary in value-based outcomes models for infected TKA. Clin Orthop Relat Res 476:1940–1948. https://doi.org/10.1007/s11999.0000000000000134
Bovonratwet P, Shen TS, Ast MP, Mayman DJ, Haas SB, Su EP (2020) Reasons and risk factors for 30-day readmission after outpatient total knee arthroplasty: a review of 3015 cases. J Arthroplasty 35:2451–2457. https://doi.org/10.1016/j.arth.2020.04.073
Mahajan SM, Nguyen C, Bui J, Kunde E, Abbott BT, Mahajan AS (2020) Risk factors for readmission after knee arthroplasty based on predictive models: a systematic review. Arthroplasty Today 6:390–404. https://doi.org/10.1016/j.artd.2020.04.017
Suganyadevi S, Seethalakshmi V, Balasamy K (2022) A review on deep learning in medical image analysis. Int J Multimed Info Retr 11:19–38. https://doi.org/10.1007/s13735-021-00218-1
Klemt C, Tirumala V, Habibi Y, Buddhiraju A, Chen TL-W, Kwon Y-M (2022) The utilization of artificial neural networks for the prediction of 90-day unplanned readmissions following total knee arthroplasty. Arch Orthop Trauma Surg. https://doi.org/10.1007/s00402-022-04566-3
Klemt C, Uzosike AC, Harvey MJ, Laurencin S, Habibi Y, Kwon Y-M (2022) Neural network models accurately predict discharge disposition after revision total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 30:2591–2599. https://doi.org/10.1007/s00167-021-06778-3
Martin RK, Ley C, Pareek A, Groll A, Tischer T, Seil R (2022) Artificial intelligence and machine learning: an introduction for orthopaedic surgeons. Knee Surg Sports Traumatol Arthrosc 30:361–364. https://doi.org/10.1007/s00167-021-06741-2
Mohammadi R, Jain S, Namin AT, Scholem Heller M, Palacholla R, Kamarthi S, Wallace B (2020) Predicting unplanned readmissions following a hip or knee arthroplasty: retrospective observational study. JMIR Med Inform 8:e19761. https://doi.org/10.2196/19761
Buddhiraju A, Chen TL-W, Subih MA, Seo HH, Esposito JG, Kwon Y-M (2023) Validation and generalizability of machine learning models for the prediction of discharge disposition following revision total knee arthroplasty. J Arthroplasty S0883–5403(23):00185–00187. https://doi.org/10.1016/j.arth.2023.02.054
Klemt C, Tirumala V, Barghi A, Cohen-Levy WB, Robinson MG, Kwon Y-M (2022) Artificial intelligence algorithms accurately predict prolonged length of stay following revision total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 30:2556–2564. https://doi.org/10.1007/s00167-022-06894-8
Klemt C, Laurencin S, Uzosike AC, Burns JC, Costales TG, Yeo I, Habibi Y, Kwon Y-M (2022) Machine learning models accurately predict recurrent infection following revision total knee arthroplasty for periprosthetic joint infection. Knee Surg Sports Traumatol Arthrosc 30:2582–2590. https://doi.org/10.1007/s00167-021-06794-3
Lopez CD, Gazgalis A, Boddapati V, Shah RP, Cooper HJ, Geller JA (2021) Artificial learning and machine learning decision guidance applications in total hip and knee arthroplasty: a systematic review. Arthroplasty Today 11:103–112. https://doi.org/10.1016/j.artd.2021.07.012
Kunze KN, Orr M, Krebs V, Bhandari M, Piuzzi NS (2022) Potential benefits, unintended consequences, and future roles of artificial intelligence in orthopaedic surgery research : a call to emphasize data quality and indications. Bone Jt Open 3:93–97. https://doi.org/10.1302/2633-1462.31.BJO-2021-0123.R1
Abbas A, Mosseri J, Lex JR, Toor J, Ravi B, Khalil EB, Whyne C (2022) Machine learning using preoperative patient factors can predict duration of surgery and length of stay for total knee arthroplasty. Int J Med Informatics 158:104670. https://doi.org/10.1016/j.ijmedinf.2021.104670
Harris AHS, Kuo AC, Weng Y, Trickey AW, Bowe T, Giori NJ (2019) Can machine learning methods produce accurate and easy-to-use prediction models of 30-day complications and mortality after knee or hip arthroplasty? Clin Orthop Relat Res 477:452–460. https://doi.org/10.1097/CORR.0000000000000601
Hyer MJ, White S, Cloyd J, Dillhoff M, Tsung A, Pawlik TM, Ejaz A (2020) Can we improve prediction of adverse surgical outcomes? Development of a surgical complexity score using a novel machine learning technique. Journal of the American College of Surgeons 230:43-52e1. https://doi.org/10.1016/j.jamcollsurg.2019.09.015
Ramkumar PN, Navarro SM, Haeberle HS, Karnuta JM, Mont MA, Iannotti JP, Patterson BM, Krebs VE (2019) Development and validation of a machine learning algorithm after primary total hip arthroplasty: applications to length of stay and payment models. J Arthroplasty 34:632–637. https://doi.org/10.1016/j.arth.2018.12.030
Shiloach M, Frencher SK, Steeger JE, Rowell KS, Bartzokis K, Tomeh MG, Richards KE, Ko CY, Hall BL (2010) Toward robust information: data quality and inter-rater reliability in the American College of Surgeons National Surgical Quality Improvement Program. J Am Coll Surg 210:6–16. https://doi.org/10.1016/j.jamcollsurg.2009.09.031
Sloan M, Sheth N, Lee G-C (2019) Is obesity associated with increased risk of deep vein thrombosis or pulmonary embolism after hip and knee arthroplasty? A large database study. Clin Orthop Relat Res 477:523–532. https://doi.org/10.1097/CORR.0000000000000615
Bhandari M, Smith J, Miller LE, Block JE (2012) Clinical and economic burden of revision knee arthroplasty. Clin Med Insights Arthritis Musculoskelet Disord 5:89–94. https://doi.org/10.4137/CMAMD.S10859
Chen TL-W, Buddhiraju A, Seo HH, Subih MA, Tuchinda P, Kwon Y-M (2023) Internal and external validation of the generalizability of machine learning algorithms in predicting non-home discharge disposition following primary total knee joint arthroplasty. J Arthroplasty S0883–5403(23):00085–00092. https://doi.org/10.1016/j.arth.2023.01.065
Chiasakul T, Buckner TW, Li M, Vega R, Gimotty PA, Cuker A (2020) In-hospital complications and readmission in patients with hemophilia undergoing hip or knee arthroplasty. JBJS Open Access 5:e0085–e0085. https://doi.org/10.2106/JBJS.OA.19.00085
Zawadzki N, Wang Y, Shao H, Liu E, Song C, Schoonmaker M, Shi L (2017) Readmission due to infection following total hip and total knee procedures: a retrospective study. Medicine 96:e7961. https://doi.org/10.1097/MD.0000000000007961
Darst BF, Malecki KC, Engelman CD (2018) Using recursive feature elimination in random forest to account for correlated variables in high dimensional data. BMC Genet 19:65. https://doi.org/10.1186/s12863-018-0633-8
Mandrekar JN (2010) Receiver operating characteristic curve in diagnostic test assessment. J Thorac Oncol 5:1315–1316. https://doi.org/10.1097/JTO.0b013e3181ec173d
Chen TL-W, Buddhiraju A, Costales TG, Subih MA, Seo HH, Kwon Y-M (2023) Machine learning models based on a national-scale cohort identify patients at high risk for prolonged lengths of stay following primary total hip arthroplasty. The Journal of Arthroplasty S0883540323006472. https://doi.org/10.1016/j.arth.2023.06.009
Wang Z, Wu C, Zheng K, Niu X, Wang X (2019) SMOTETomek-based resampling for personality recognition. IEEE Access 7:129678–129689. https://doi.org/10.1109/ACCESS.2019.2940061
Montesinos López OA, Montesinos López A, Crossa J (2022) Fundamentals of artificial neural networks and deep learning. In: Montesinos López OA, Montesinos López A, Crossa J (eds) Multivariate statistical machine learning methods for genomic prediction, 1st edn. Springer International Publishing, Cham, pp 379–425
Svetnik V, Liaw A, Tong C, Culberson JC, Sheridan RP, Feuston BP (2003) Random forest: a classification and regression tool for compound classification and QSAR modeling. J Chem Inf Comput Sci 43:1947–1958. https://doi.org/10.1021/ci034160g
Guryanov A (2019) Histogram-based algorithm for building gradient boosting ensembles of piecewise linear decision trees. In: van der Aalst WMP, Batagelj V, Ignatov DI, Khachay M, Kuskova V, Kutuzov A, Kuznetsov SO, Lomazova IA, Loukachevitch N, Napoli A, Pardalos PM, Pelillo M, Savchenko AV, Tutubalina E (eds) Analysis of images, social networks and texts. Springer International Publishing, Cham, pp 39–50
Kramer O (2013) K-Nearest Neighbors. In: Kramer O (ed) Dimensionality reduction with unsupervised nearest neighbors. Springer, Berlin, Heidelberg, pp 13–23
Jones CD, Falvey J, Hess E, Levy CR, Nuccio E, Barón AE, Masoudi FA, Stevens-Lapsley J (2019) Predicting hospital readmissions from home healthcare in medicare beneficiaries. J Am Geriatr Soc 67:2505–2510. https://doi.org/10.1111/jgs.16153
Mohammed H, Huang Y, Memtsoudis S, Parks M, Huang Y, Ma Y (2022) Utilization of machine learning methods for predicting surgical outcomes after total knee arthroplasty. PLoS ONE 17:e0263897. https://doi.org/10.1371/journal.pone.0263897
Zhong H, Poeran J, Gu A, Wilson LA, Gonzalez Della Valle A, Memtsoudis SG, Liu J (2021) Machine learning approaches in predicting ambulatory same day discharge patients after total hip arthroplasty. Reg Anesth Pain Med 46:779–783. https://doi.org/10.1136/rapm-2021-102715
Wong J, Manderson T, Abrahamowicz M, Buckeridge DL, Tamblyn R (2019) Can hyperparameter tuning improve the performance of a super learner?: a case study. Epidemiology 30:521–531. https://doi.org/10.1097/EDE.0000000000001027
Steyerberg EW, Vickers AJ, Cook NR, Gerds T, Gonen M, Obuchowski N, Pencina MJ, Kattan MW (2010) Assessing the performance of prediction models: a framework for traditional and novel measures. Epidemiology 21:128–138. https://doi.org/10.1097/EDE.0b013e3181c30fb2
Stevens RJ, Poppe KK (2020) Validation of clinical prediction models: what does the “calibration slope” really measure? J Clin Epidemiol 118:93–99. https://doi.org/10.1016/j.jclinepi.2019.09.016
Vickers AJ, Elkin EB (2006) Decision curve analysis: a novel method for evaluating prediction models. Med Decis Making 26:565–574. https://doi.org/10.1177/0272989X06295361
Hinterwimmer F, Lazic I, Langer S, Suren C, Charitou F, Hirschmann MT, Matziolis G, Seidl F, Pohlig F, Rueckert D, Burgkart R, von Eisenhart-Rothe R (2023) Prediction of complications and surgery duration in primary TKA with high accuracy using machine learning with arthroplasty-specific data. Knee Surg Sports Traumatol Arthrosc 31:1323–1333. https://doi.org/10.1007/s00167-022-06957-w
Kim JH, Kwon YS, Baek MS (2021) Machine learning models to predict 30-day mortality in mechanically ventilated patients. JCM 10:2172. https://doi.org/10.3390/jcm10102172
Kunze KN, Polce EM, Sadauskas AJ, Levine BR (2020) Development of machine learning algorithms to predict patient dissatisfaction after primary total knee arthroplasty. J Arthroplasty 35:3117–3122. https://doi.org/10.1016/j.arth.2020.05.061
Van Onsem S, Verstraete M, Dhont S, Zwaenepoel B, Van Der Straeten C, Victor J (2018) Improved walking distance and range of motion predict patient satisfaction after TKA. Knee Surg Sports Traumatol Arthrosc 26:3272–3279. https://doi.org/10.1007/s00167-018-4856-z
Steyerberg EW, Vergouwe Y (2014) Towards better clinical prediction models: seven steps for development and an ABCD for validation. Eur Heart J 35:1925–1931. https://doi.org/10.1093/eurheartj/ehu207
Aram P, Trela-Larsen L, Sayers A, Hills AF, Blom AW, McCloskey EV, Kadirkamanathan V, Wilkinson JM (2018) Estimating an individual’s probability of revision surgery after knee replacement: a comparison of modeling approaches using a national data set. Am J Epidemiol 187:2252–2262. https://doi.org/10.1093/aje/kwy121
Kurtz SM, Lau EC, Ong KL, Adler EM, Kolisek FR, Manley MT (2016) Which hospital and clinical factors drive 30- and 90-day readmission after TKA? J Arthroplasty 31:2099–2107. https://doi.org/10.1016/j.arth.2016.03.045
Williams CL, Pujalte G, Li Z, Vomer RP, Nishi M, Kieneker L, Ortiguera CJ (2022) Which factors predict 30-day readmission after total hip and knee replacement surgery? Cureus. https://doi.org/10.7759/cureus.23093
He H, Garcia EA (2009) Learning from imbalanced data. IEEE Trans Knowl Data Eng 21:1263–1284. https://doi.org/10.1109/TKDE.2008.239
Li L, Wang L, Lu L, Zhu T (2022) Machine learning prediction of postoperative unplanned 30-day hospital readmission in older adult. Front Mol Biosci 9:910688. https://doi.org/10.3389/fmolb.2022.910688
Umer M, Sadiq S, Missen MMS, Hameed Z, Aslam Z, Siddique MA, Nappi M (2021) Scientific papers citation analysis using textual features and SMOTE resampling techniques. Pattern Recogn Lett 150:250–257. https://doi.org/10.1016/j.patrec.2021.07.009
Benito J, Stafford J, Judd H, Ng M, Corces A, Roche MW (2022) Length of stay increases 90-day readmission rates in patients undergoing primary total joint arthroplasty. JAAOS Glob Res Rev 6. https://doi.org/10.5435/JAAOSGlobal-D-21-00271
Lehtonen EJ, Hess MC, McGwin G, Shah A, Godoy-Santos AL, Naranje S (2018) Risk factors for early hospital readmission following total knee arthroplasty. Acta Ortop Bras 26:309–313. https://doi.org/10.1590/1413-785220182605190790
Siracuse BL, Ippolito JA, Gibson PD, Ohman-Strickland PA, Beebe KS (2017) A preoperative scale for determining surgical readmission risk after total knee arthroplasty. J Bone Joint Surg Am 99:e112. https://doi.org/10.2106/JBJS.16.01043
Alzubi J, Nayyar A, Kumar A (2018) Machine learning from theory to algorithms: an overview. J Phys: Conf Ser 1142:012012. https://doi.org/10.1088/1742-6596/1142/1/012012
Novack TA, Kurowicki J, Issa K, Pierce TP, Festa A, McInerney VK, Scillia AJ (2020) Accelerated discharge following total knee arthroplasty may be safe in a teaching institution. J Knee Surg 33:8–11. https://doi.org/10.1055/s-0038-1676066
Sutton JC, Antoniou J, Epure LM, Huk OL, Zukor DJ, Bergeron SG (2016) Hospital discharge within 2 days following total hip or knee arthroplasty does not increase major-complication and readmission rates. J Bone Joint Surg Am 98:1419–1428. https://doi.org/10.2106/JBJS.15.01109
Jeon CY, Neidell M, Jia H, Sinisi M, Larson E (2012) On the role of length of stay in healthcare-associated bloodstream infection. Infect Control Hosp Epidemiol 33:1213–1218. https://doi.org/10.1086/668422
Dahlgren N, Lehtonen E, Anderson M, Archie AT, McGwin G, Shah A, Naranje SM (2018) Readmission following revision total knee arthroplasty: an institutional cohort. Cureus. https://doi.org/10.7759/cureus.3640
Khoshbin A, Hoit G, Nowak LL, Daud A, Steiner M, Juni P, Ravi B, Atrey A (2021) The association of preoperative blood markers with postoperative readmissions following arthroplasty. Bone Joint Open 2:388–396. https://doi.org/10.1302/2633-1462.26.BJO-2021-0020
Arroyo NS, White RS, Gaber-Baylis LK, La M, Fisher AD, Samaru M (2019) Racial/ethnic and socioeconomic disparities in total knee arthroplasty 30- and 90-day readmissions: a multi-payer and multistate analysis, 2007–2014. Popul Health Manag 22:175–185. https://doi.org/10.1089/pop.2018.0025
Elsiwy Y, Jovanovic I, Doma K, Hazratwala K, Letson H (2019) Risk factors associated with cardiac complication after total joint arthroplasty of the hip and knee: a systematic review. J Orthop Surg Res 14:15. https://doi.org/10.1186/s13018-018-1058-9
van Rensch PJH, Hannink G, Heesterbeek PJC, Wymenga AB, van Hellemondt GG (2020) Long-term outcome following revision total knee arthroplasty is associated with indication for revision. J Arthroplasty 35:1671–1677. https://doi.org/10.1016/j.arth.2020.01.053
Zajonz D, Höhn C, Neumann J, Angrick C, Möbius R, Huschak G, Neumuth T, Ghanem M, Roth A (2020) Increasing efficiency by optimizing table position for elective primary THA and TKA: a prospective monocentric pilot study. Arthroplasty 2:29. https://doi.org/10.1186/s42836-020-00048-2
Chan VW, Chan P, Fu H, Cheung M, Cheung A, Yan C, Chiu K (2020) Preoperative optimization to prevent periprosthetic joint infection in at-risk patients. J Orthop Surg (Hong Kong) 28:230949902094720. https://doi.org/10.1177/2309499020947207
Hamilton DF, Burnett R, Patton JT, Howie CR, Moran M, Simpson AHRW, Gaston P (2015) Implant design influences patient outcome after total knee arthroplasty: a prospective double-blind randomised controlled trial. Bone Joint J 97:64–70. https://doi.org/10.1302/0301-620X.97B1.34254
Wan X, Yang Y, Wang D, Xu H, Huang C, Zhou Z, Xu J (2022) Comparison of outcomes after total knee arthroplasty involving postoperative neutral or residual mild varus alignment: a systematic review and meta-analysis. Orthop Surg 14:177–189. https://doi.org/10.1111/os.13155
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.

Fig. 4
The receiver operating characteristic curve produced by A) artificial neural network, B) random forest, C) histogram-based gradient boosting, and D) k-nearest neighbors during training. The results are averaged across the five-fold cross-validation. Solid lines represent the mean values. Dash lines and the gray area in between indicate the standard deviations. (PNG 662 kb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chen, T.LW., Shimizu, M.R., Buddhiraju, A. et al. Predicting 30-day unplanned hospital readmission after revision total knee arthroplasty: machine learning model analysis of a national patient cohort. Med Biol Eng Comput 62, 2073–2086 (2024). https://doi.org/10.1007/s11517-024-03054-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-024-03054-7