Abstract
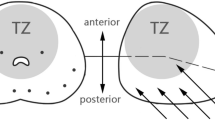
Objectives This paper aims to provide an explanation for the positive findings of the improved prostate cancer detection rate by the transperineal approach when compared to the transrectal approach. The peripheral zone (PZ) is a region of the prostate with the most cancer occurrence. Hence, the ability to reach it consistently can improve the cancer detection rate significantly.
Methods In a prospective study, ultrasound images taken from five patients were used to reconstruct the prostate, rectum and pubic bone with the perineal wall data obtained from the same patient. Each anatomical model virtually underwent prostate biopsy transperineally and transrectally with 10 cores biopsy each. We assessed the efficacy by calculating the volume of PZ tissue obtained from each approach.
Results The overall volume of virtual core tissue taken from the PZ was 81.7% from a total volume of 100 prostate biopsy cores. Of the volume of tissue extracted transperineally, 98.5% was from the PZ compared to only 64.9% of the transrectally extracted tissue.
Conclusions This is the first paper that acquires and reconstructs the virtual anatomy of the prostate, rectum and pubic bone with the perineal wall. Transperineal biopsy is superior to the transrectal method in obtaining the peripheral zone tissue. This explains the findings that the prostate cancer detection rate is higher via the transperineal approach.
Similar content being viewed by others
References
Applewhite JC, Matlaga BR, McCullough DL, Craig Hall M (2001) Transrectal ultrasound and biopsy in the early diagnosis of prostate cancer. Cancer Control 8(2):141–150
Raja J, Ramachandran N, Munneke G, Patel U (2006) Current status of transrectal ultrasound-guided prostate biopsy in the diagnosis of prostate cancer. Clin Radiol 61:142–153
Moussa M (2005) Diagnostic and systemic pathology: genitourinary, prostate gland. London Health Sciences Centre, University Campus, Canada
Pinkstaff DM, Igel TC, Petrou SP, Broderick GA, Wehle MJ, Young PR (2003) Systematic transperineal ultrasound-guided template biopsy of the prostate: three year experience. Urology 65:735–739
Frimmel H, Egevad L, Bengtsson E et al (1999) Modeling prostate cancer distribution. Urology 54:1028–1034
Kabalin JN, McNeal JE, Price HM et al (1989) Unsuspected adenocarcinoma of the prostate in patients undergoing cystoprostatectomy for other causes: incidence, histology and morphometric observations. J Urol 141:1091–1094
McNeal JE, Redwine EA, Freiha FS, Stamey TA (1988) Zonal distribution of prostatic adenocarcinoma. Correlation with histologic pattern and direction of spread. Am J Surg Pathol 12:897–906
Flanigan RC, Catalona WJ, Richie JP, Ahmann FR, Hudson MA, Scardino RC, DeKernion JB, Fatliff TL, Kavoussi LR, Dalkin BL, Waters WB, MacFarlance MT, Southwick PC (1994) Accuracy of digital rectal examination and transrectal ultrasonography in localizing prostate cancer. J Urol 152:1506–1509
Emiliozzi P, Corsetti A, Tassi B, Federico G, Martini M, Pansadoro V (2003) Best approach for prostate cancer detection: a prospective study on transperineal versus transrectal six core prostate biopsy. Urology 61:961–965
Vis AN, Boerma MO, Ciatto S, et al (2000) Detection of prostate cancer: a comparative study of the diagnostic efficacy of sextant transrectal versus sextant transperineal biopsy. Urology 56:617–621
Watanabe M, Hayashi T, Tsushima T, Irie S, Kaneshige T, Kumon H (2005) Extensive biopsy using a combined transperineal and transrectal approach to improve prostate cancer detection. Int J Urol 12:959–963
Egevad L, Frimmel H, Norberg M, Mattson S, Carlbom I, Bengtsson E, Busch C (1999) Three-dimensional computer reconstruction of prostate cancer from radical prostatectomy specimens: evaluation of the model by core biopsy simulation. Urology 53:192–198
DigiclopsTM Stereo Vision System Installation Guide and Camera Control API Command Reference Version 2.3. (2001) Point Grey Research, Inc.
Ser E (2006) Pelvic floor reconstruction. Msc , Computer Integrated Medical Intervention Laboratory (CIMIL), Nanyang Technological University, Singapore
Wu RY (2002) Bubble 3D: a Java application for handling surfaces in volumetric medical images. Technical report, Computer Integrated Medical Intervention Laboratory (CIMIL), Nanyang Technological University, Singapore
SolidWorks® (2006) SP 4.1 Education Edition
Robb RA (2002) Three-dimensional visualization and analysis in prostate cancer. Med Actual 38:153–165
Zeng J, Kaplan C, Xuan J, Sesterhenn IA, Lynch JH, Freedman MT, Mun SK (1998) Optimizing prostate needle biopsy through 3-D simulation. SPIE 3335:488–497
Serfling R, Shulman M, Thompson GL, Xiao Z, Benaim E, Roehrborn CG, Rittmaster R (2006) Modeling prostate cancer detection probability using prostate specific antigen, transition and peripheral zone volumes, and numbers of biopsy cores. University of Texas, Dallas
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mohan, P., Ho, H., Yuen, J. et al. A 3D computer simulation to study the efficacy of transperineal versus transrectal biopsy of the prostate. Int J CARS 1, 351–360 (2007). https://doi.org/10.1007/s11548-007-0069-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-007-0069-5