Abstract
Purpose
Ultrasonography has the potential to accurately stage breast cancer with automated analysis to detect axillary lymph node metastasis. The aim of this study was to develop and test automated quantitative ultrasound image analysis of axillary lymph nodes for breast cancer staging.
Methods
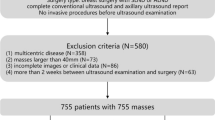
Following an IRB-approved HIPAA compliant protocol, ultrasound images of 90 breast cancer patients presenting for lymph node assessment were retrospectively collected. There were 51 node-positive and 39 node-negative patients, yielding images of 223 lymph nodes (109 positive for metastasis and 114 negative for metastasis). The analysis was completely automated apart from the manual indication of the approximate center of each lymph node. Mathematical descriptors of the nodes, which served as image-based biomarkers, were computer-extracted and input to a classifier for the task of distinguishing between positive (i.e., metastatic) and negative lymph nodes. The performance of this task was assessed using receiver operating characteristic (ROC) analysis with evaluation by-node and by-patient using the area under the ROC curve (AUC) as the performance metric.
Results
The AUC was 0.85 (standard error 0.03) for by-node evaluation when distinguishing between positive and negative lymph nodes. The AUC was 0.87 (0.04) for patient-based prognosis, i.e., assessing whether patients were lymph node-positive or lymph node-negative.
Conclusion
Based on these classification results, we conclude that mathematical descriptors of sonographically imaged lymph nodes may be useful as prognostic biomarkers in breast cancer staging and demonstrate potential for predicting patient lymph node status.





Similar content being viewed by others
References
Siegel R, Naishadham D, Jemal A (2012) Cancer statistics, 2012. CA Cancer J Clin 62(1):10–29. doi:10.3322/caac.20138
Abe H, Schmidt RA, Shah RN, Shimauchi A, Kulkarni K, Sennett CA, Newstead GM (2010) MR-directed (“Second-Look”) ultrasound examination for breast lesions detected initially on MRI: MR and sonographic findings. AJR Am J Roentgenol 194(2):370–377. doi:10.2214/AJR.09.2707
Carbognin G, Girardi V, Calciolari C, Brandalise A, Bonetti F, Russo A, Pozzi Mucelli R (2010) Utility of second-look ultrasound in the management of incidental enhancing lesions detected by breast MR imaging. Radiol Med 115(8):1234–1245. doi:10.1007/s11547-010-0561-9
Laguna AD, Arranz SJ, Checa VQ, Roca SA, Jimenez DE, Oliver-Goldaracena J (2011) Sonographic findings of additional malignant lesions in breast carcinoma seen by second look ultrasound. J Clin Imaging Sci 1:34. doi:10.4103/2156-7514.82338
Leung JW (2011) Utility of second-look ultrasound in the evaluation of MRI-detected breast lesions. Semin Roentgenol 46(4):260–274. doi:10.1053/j.ro.2011.08.002
Luciani ML, Pediconi F, Telesca M, Vasselli F, Casali V, Miglio E, Passariello R, Catalano C (2011) Incidental enhancing lesions found on preoperative breast MRI: management and role of second-look ultrasound. Radiol Med 116(6):886–904. doi:10.1007/s11547-011-0630-8
Cox CE, Cox JM, White LB, Stowell NG, Clark JD, Allred N, Meyers M, Dupont E, Furman B, Minton S (2006) Sentinel node biopsy before neoadjuvant chemotherapy for determining axillary status and treatment prognosis in locally advanced breast cancer. Ann Surg Oncol 13(4):483–490. doi:10.1245/ASO.2006.03.592
Swenson KK, Nissen MJ, Ceronsky C, Swenson L, Lee MW, Tuttle TM (2002) Comparison of side effects between sentinel lymph node and axillary lymph node dissection for breast cancer. Ann Surg Oncol 9(8):745–753
Fraile M, Rull M, Julian FJ, Fuste F, Barnadas A, Llatjos M, Castella E, Gonzalez JR, Vallejos V, Alastrue A, Broggi MA (2000) Sentinel node biopsy as a practical alternative to axillary lymph node dissection in breast cancer patients: an approach to its validity. Ann Oncol 11(6):701–705
Fisher B, Jeong JH, Anderson S, Bryant J, Fisher ER, Wolmark N (2002) Twenty-five-year follow-up of a randomized trial comparing radical mastectomy, total mastectomy, and total mastectomy followed by irradiation. N Engl J Med 347(8):567–575. doi:10.1056/NEJMoa020128
Edge SB, Niland JC, Bookman MA, Theriault RL, Ottesen R, Lepisto E, Weeks JC (2003) Emergence of sentinel node biopsy in breast cancer as standard-of-care in academic comprehensive cancer centers. J Natl Cancer Inst 95(20):1514–1521
Giuliano AE, McCall L, Beitsch P, Whitworth PW, Blumencranz P, Leitch AM, Saha S, Hunt KK, Morrow M, Ballman K (2010) Locoregional recurrence after sentinel lymph node dissection with or without axillary dissection in patients with sentinel lymph node metastases: the American College of Surgeons Oncology Group Z0011 randomized trial. Ann Surg 252(3):426–432; discussion 432–423 doi:10.1097/SLA.0b013e3181f08f32
Lucci A, McCall LM, Beitsch PD, Whitworth PW, Reintgen DS, Blumencranz PW, Leitch AM, Saha S, Hunt KK, Giuliano AE (2007) Surgical complications associated with sentinel lymph node dissection (SLND) plus axillary lymph node dissection compared with SLND alone in the American college of surgeons oncology group trial Z0011. J Clin Oncol 25(24):3657–3663. doi:10.1200/JCO.2006.07.4062
Deurloo EE, Tanis PJ, Gilhuijs KG, Muller SH, Kroger R, Peterse JL, Rutgers EJ, Valdes Olmos R, Schultze Kool LJ (2003) Reduction in the number of sentinel lymph node procedures by preoperative ultrasonography of the axilla in breast cancer. Eur J Cancer 39(8):1068–1073
Cho N, Moon WK, Han W, Park IA, Cho J, Noh DY (2009) Preoperative sonographic classification of axillary lymph nodes in patients with breast cancer: node-to-node correlation with surgical histology and sentinel node biopsy results. AJR Am J Roentgenol 193(6):1731–1737. doi:10.2214/AJR.09.3122
Yang WT, Chang J, Metreweli C (2000) Patients with breast cancer: differences in color Doppler flow and gray-scale US features of benign and malignant axillary lymph nodes. Radiology 215(2):568–573
Abe H, Schmidt RA, Kulkarni K, Sennett CA, Mueller JS, Newstead GM (2009) Axillary lymph nodes suspicious for breast cancer metastasis: sampling with US-guided 14-gauge core-needle biopsy-clinical experience in 100 patients. Radiology 250(1): 41–49. doi:10.1148/radiol.2493071483
Alvarez S, Anorbe E, Alcorta P, Lopez F, Alonso I, Cortes J (2006) Role of sonography in the diagnosis of axillary lymph node metastases in breast cancer: a systematic review. AJR Am J Roentgenol 186(5):1342–1348. doi:10.2214/AJR.05.0936
Giger ML, Chan HP, Boone J (2008) Anniversary paper: History and status of CAD and quantitative image analysis: the role of medical physics and AAPM. Med Phys 35(12):5799–5820
Shiraishi J, Li Q, Appelbaum D, Doi K (2011) Computer-aided diagnosis and artificial intelligence in clinical imaging. Semin Nucl Med 41(6):462. doi:10.1053/j.semnuclmed.2011.06.004
Bhooshan N, Giger M, Edwards D, Yuan Y, Jansen S, Li H, Lan L, Sattar H, Newstead G (2011) Computerized three-class classification of MRI-based prognostic markers for breast cancer. Phys Med Biol 56(18):5995–6008. doi:10.1088/0031-9155/56/18/014
Bhooshan N, Giger ML, Jansen SA, Li H, Lan L, Newstead GM (2010) Cancerous breast lesions on dynamic contrast-enhanced MR images: computerized characterization for image-based prognostic markers. Radiology 254(3):680–690. doi:10.1148/radiol.09090838
Kim MH, Kim JK, Lee Y, Park BW, Lee CK, Kim N, Cho G, Choi HJ, Cho KS (2011) Diagnosis of lymph node metastasis in uterine cervical cancer: usefulness of computer-aided diagnosis with comprehensive evaluation of MR images and clinical findings. Acta Radiol 52(10):1175–1183. doi:10.1258/ar.2011.110202
Zhang J, Wang Y, Dong Y (2008) Computer-aided diagnosis of cervical lymph nodes on ultrasonography. Comput Biol Med 38(2):234–243. doi:10.1016/j.compbiomed.2007.10.005
Cui C, Cai H, Liu L, Li L, Tian H (2011) Quantitative analysis and prediction of regional lymph node status in rectal cancer based on computed tomography imaging. Eur Radiol 21(11):2318–2325. doi:10.1007/s00330-011-2182-7
Horsch K, Giger ML, Venta LA, Vyborny CJ (2001) Automatic segmentation of breast lesions on ultrasound. Med Phys 28(8): 1652–1659
Glantz SA (2005) Primer of biostatistics. McGraw-Hill Professional, New York
Gruszauskas NP, Drukker K, Giger ML, Sennett CA, Pesce LL (2008) Performance of breast ultrasound computer-aided diagnosis: dependence on image selection. Acad Radiol 15(10):1234–1245. doi:10.1016/j.acra.2008.04.016
Horsch K, Giger ML, Venta LA, Vyborny CJ (2002) Computerized diagnosis of breast lesions on ultrasound. Med Phys 29(2):157–164
Golugula A, Lee G, Madabhushi A (2011) Evaluating feature selection strategies for high dimensional, small sample size datasets. Conf Proc IEEE Eng Med Biol Soc 2011:949–952. doi:10.1109/IEMBS.2011.6090214
Pesce LL, Metz CE (2007) Reliable and computationally efficient maximum-likelihood estimation of “proper” binormal ROC curves. Acad Radiol 14(7):814–829. doi:10.1016/j.acra.2007.03.012
Metz CE (1978) Basic principles of ROC analysis. Semin Nucl Med 8(4):283–298
Metz CE, Herman BA, Roe CA (1998) Statistical comparison of two ROC-curve estimates obtained from partially-paired datasets. Med Decis Mak 18(1):110–121
Kupinski MA, Giger ML (1998) Automated seeded lesion segmentation on digital mammograms. IEEE Trans Med Imaging 17(4):510–517
Drukker K, Horsch K, Giger ML (2005) Multimodality computerized diagnosis of breast lesions using mammography and sonography. Acad Radiol 12(8):970–979. doi:10.1016/j.acra.2005.04.014
Horsch K, Giger ML, Vyborny CJ, Lan L, Mendelson EB, Hendrick RE (2006) Classification of breast lesions with multimodality computer-aided diagnosis: observer study results on an independent clinical data set. Radiology 240(2):357–368. doi:10.1148/radiol.2401050208
Sahiner B, Chan HP, Hadjiiski LM, Roubidoux MA, Paramagul C, Bailey JE, Nees AV, Blane CE, Adler DD, Patterson SK, Klein KA, Pinsky RW, Helvie MA (2009) Multi-modality CADx: ROC study of the effect on radiologists’ accuracy in characterizing breast masses on mammograms and 3D ultrasound images. Acad Radiol 16(7):810–818. doi:10.1016/j.acra.2009.01.011
Yuan Y, Giger ML, Li H, Bhooshan N, Sennett CA (2010) Multimodality computer-aided breast cancer diagnosis with FFDM and DCE-MRI. Acad Radiol 17(9):1158–1167. doi:10.1016/j.acra.2010.04.015
Meinel LA, Abe H, Bergtholdt M, Ecanow J, Schmidt R, Newstead G (2010) Multi-modality morphological correlation of axillary lymph nodes. Int J Comput Assist Radiol Surg 5(4):343–350. doi:10.1007/s11548-010-0421-z
Drukker K, Giger ML, Metz CE (2005) Robustness of computerized lesion detection and classification scheme across different breast US platforms. Radiology 237(3):834–840. doi:10.1148/radiol.2373041418
Gruszauskas NP, Drukker K, Giger ML, Chang RF, Sennett CA, Moon WK, Pesce LL (2009) Breast US computer-aided diagnosis system: robustness across urban populations in South Korea and the United States. Radiology 253(3):661–671. doi:10.1148/radiol.2533090280
Drukker K, Pesce L, Giger M (2010) Repeatability in computer-aided diagnosis: application to breast cancer diagnosis on sonography. Med Phys 37(6):2659–2669
Jamieson AR, Giger ML, Drukker K, Li H, Yuan Y, Bhooshan N (2010) Exploring nonlinear feature space dimension reduction and data representation in breast Cadx with Laplacian eigenmaps and t-SNE. Med Phys 37(1):339–351
Cronin B, Stevenson IH, Sur M, Kording KP (2010) Hierarchical Bayesian modeling and Markov chain Monte Carlo sampling for tuning-curve analysis. J Neurophysiol 103(1):591–602. doi:10.1152/jn.00379.2009
Acknowledgments
This work was supported in part by Department of Energy grant DE-FG02-08ER6478, National Institute of Health grants NIH P50-CA125183 and NIH S10 RR021039, and a research grant from Philips Medical Research.
Conflict of iInterest
M.L.G. is a stockholder in R2 Technology/Hologic is cofounder & equity holder in Quantitative Insights, Inc., and receives royalties from Hologic, GE Medical Systems, MEDIAN Technologies, Riverain Medical, Mitsubishi and Toshiba. K.D. received royalties from Hologic. It is the University of Chicago Conflict of Interest Policy that investigators disclose publicly actual or potential significant financial interest that would reasonably appear to be directly and significantly affected by the research activities.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Drukker, K., Giger, M., Meinel, L.A. et al. Quantitative ultrasound image analysis of axillary lymph node status in breast cancer patients. Int J CARS 8, 895–903 (2013). https://doi.org/10.1007/s11548-013-0829-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-013-0829-3