Abstract
Purpose
The performance of a fusion-based needle deflection estimation method was experimentally evaluated using prostate brachytherapy phantoms. The accuracy of the needle deflection estimation was determined. The robustness of the approach with variations in needle insertion speed and soft tissue biomechanical properties was investigated.
Methods
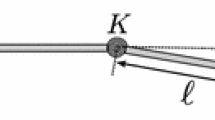
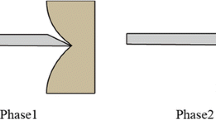
A needle deflection estimation method was developed to determine the amount of needle bending during insertion into deformable tissue by combining a kinematic deflection model with measurements taken from two electromagnetic trackers placed at the tip and the base of the needle. Experimental verification of this method for use in prostate brachytherapy needle insertion procedures was performed. A total of 21 beveled tip, 18 ga, 200 mm needles were manually inserted at various speeds through a template and toward different targets distributed within 3 soft tissue mimicking polyvinyl chloride prostate phantoms of varying stiffness. The tracked positions of both the needle tip and base were recorded, and Kalman filters were applied to fuse the sensory information. The estimation results were validated using ground truth obtained from fluoroscopy images.
Results
The manual insertion speed ranged from 8 to 34 mm/s, needle deflection ranged from 5 to 8 mm at an insertion depth of 76 mm, and the elastic modulus of the soft tissue ranged from 50 to 150 kPa. The accuracy and robustness of the estimation method were verified within these ranges. When compared to purely model-based estimation, we observed a reduction in needle tip position estimation error by \(52\pm 17\) % (mean \(\pm \) SD) and the cumulative deflection error by \(57\pm 19\) %.
Conclusions
Fusion of electromagnetic sensors demonstrated significant improvement in estimating needle deflection compared to model-based methods. The method has potential clinical applicability in the guidance of needle placement medical interventions, particularly prostate brachytherapy.







Similar content being viewed by others
References
Park W, Liu Y, Zhou Y, Moses M, Chirikjian GS (2008) Kinematic state estimation and motion planning for stochastic nonholonomic systems using the exponential map. Robotica 26(4):419–434
Abolhassani N, Patel R, Moallem M (2007) Needle insertion into soft tissue: a survey. Med Eng Phys 29(4):413–431
Sadjadi H, Hashtrudi-Zaad K, Fichtinger G (2012) Needle deflection estimation using fusion of electromagnetic trackers. In: International conference of the IEEE engineering in medicine and biology society (EMBC). San Diego, pp 952–955
Sadjadi H, Hashtrudi-Zaad K, Fichtinger G (Oct 2013) Fusion of electromagnetic trackers to improve needle deflection estimation: simulation study. IEEE Trans Biomed Eng (TBME) 60(10):2706–2715
Sadjadi H, Hashtrud-Zaad K, Xu H, Fichtinger G (2013) Experimental evaluation of needle deflection estimation for brachytherapy. In: Computer assisted radiology and surgery (CARS 2013). Heidelberg (abstract in International Journal of Computer Assisted Surgery and Radiology, 8(1):391–392)
Hinnen KA, Battermann JJ, van Roermund JGH, Moerland MA, Jurgenliemk-Schulz IM, Frank SJ, van Vulpen M (2010) Long-term biochemical and survival outcome of 921 patients treated with I-125 permanent prostate brachytherapy. Int J Radiat Oncol Biol Phys 76(5):1433–1438
Wallner K, Merrick G, Dattoli MJ, Blasko JC (2007) Prostate brachytherapy made complicated. SmartMedicine Press, p 600
Van Veen YRJ, Jahya A, Misra S (2012) Macroscopic and microscopic observations of needle insertion into gels. Eng Med 226(6):441–449
Podder T, Clark D, Sherman J, Fuller D, Messing E, Rubens D, Strang J, Zhang Y, O’Dell W, Ng W, Yu Y (2005) Effects of tip geometry of surgical needles: an assessment of force and deflection. In: European medical and biological engineering conference (EMBEC05). Prague, pp 1727–1983
Podder T, Sherman J, Rubens D, Messing E, Strang J, Ng WS, Yu Y (2008) Methods for prostate stabilization during transperineal LDR brachytherapy. Phys Med Biol 53(6):1563
Nath S, Chen Z, Yue N, Trumpore S, Peschel R (2000) Dosimetric effects of needle divergence in prostate seed implant using 125I and 103Pd radioactive seeds. Med Phys 27(5):1058
Lagerburg V, Moerland M, Konings M, Vosse R, JaBJ Lagendijk (2006) Development of a tapping device: a new needle insertion method for prostate brachytherapy. Phys Med Biol 51:891
Abolhassani N, Patel R, Ayazi F (2007) Effects of different insertion methods on reducing needle deflection. In: 29th Annual international conference of the IEEE engineering in medicine and biology society, EMBS 2007, pp 491–494
McGill CS, Schwartz JA, Moore JZ, McLaughlin PW, Shih AJ (2011) Precision grid and hand motion for accurate needle insertion in brachytherapy. Med Phys 38:4749
Majewicz A, Marra S, van Vledder M, Lin M, Choti M, Song D, Okamura A (2012) Behavior of tip-steerable needles in ex vivo and in vivo tissue. IEEE Trans Biomed Eng 59(10):2705–2715
Goksel O, Dehghan E, Salcudean S (2009) Modeling and simulation of flexible needles. Med Eng Phys 31(9):1069–1078
Glozman D, Shoham M (2007) Image-guided robotic flexible needle steering. IEEE Trans Robot 23(3):459–467
Asadian A, Kermani M, Patel R (2011) An analytical model for deflection of flexible needles during needle insertion. In: IEEE/RSJ international conference on intelligent robots and systems (IROS), pp 2551–2556
Okamura AM, Simone C, O’Leary MD (2004) Force modeling for needle insertion into soft tissue. IEEE Trans Biomed Eng 51(10):1707–1716
DiMaio SP, Salcudean S (2003) Needle insertion modeling and simulation. IEEE Trans Robot Autom 19(5):864–875
Podder T, Clark D, Sherman J, Fuller D, Messing E, Rubens D, Strang J, Brasacchio R, Liao L, Ng WS et al (2006) In vivo motion and force measurement of surgical needle intervention during prostate brachytherapy. Med Phys 33:2915
Yan K, Podder T, Xiao D, Yu Y, Liu TI, Cheng C, Ng W (2006) An improved needle steering model with online parameter estimator. Int J Comput Assist Radiol Surg 1(4):205–212
Jafari AH, Dhaouadi R, Jhemi A (2013) Nonlinear friction estimation in elastic drive systems using a dynamic neural network-based observer. J Adv Comput Intell Intell Inform 17(4):637–646
DiMaio SP, Salcudean SE (2005) Needle steering and motion planning in soft tissues. IEEE Trans Biomed Eng 52(6):965–974
Webster RJ, Kim JS, Cowan NJ, Chirikjian GS, Okamura AM (2006) Nonholonomic modeling of needle steering. Int J Robot Res 25(5):509
Minhas DS, Engh JA, Fenske MM, Riviere CN (2007) Modeling of needle steering via duty-cycled spinning. In: International conference of the IEEE engineering in medicine and biology society (EMBC), pp 2756–2759
Bernardes MC, Adorno BV, Poignet P, Borges GA (2013) Robot-assisted automatic insertion of steerable needles with closed-loop imaging feedback and intraoperative trajectory replanning. Mechatronics 23(6):630–645
Park W, Reed KB, Okamura AM, Chirikjian GS (2010) Estimation of model parameters for steerable needles. In: IEEE International conference on robotics and automation (ICRA), pp 3703–3708
Maier-Hein L, Franz A, Birkfellner W, Hummel J, Gergel I, Wegner I, Meinzer HP (2012) Standardized assessment of new electromagnetic field generators in an interventional radiology setting. Med Phys 39:3424
Aboofazeli M, Abolmaesumi P, Mousavi P, Fichtinger G (2009) A new scheme for curved needle segmentation in three-dimensional ultrasound images. In: IEEE international symposium on biomedical imaging: from nano to macro, (ISBI), pp 1067–1070
Ren H, Rank D, Merdes M, Stallkamp J, Kazanzides P (2012) Multisensor data fusion in an integrated tracking system for endoscopic surgery. IEEE Trans Inf Technol Biomed 16(1):106–111
Dehghan E, Wen X, Zahiri-Azar R, Marchal M, Salcudean SE (2008) Needle-tissue interaction modeling using ultrasound-based motion estimation: phantom study. Computer Aided Surg 13(5):265–280
Datla NV, Konh B, Koo JJ, Choi DJ, Yu Y, Dicker AP, Podder TK, Darvish K, Hutapea P (2014) Polyacrylamide phantom for self-actuating needle-tissue interaction studies. Med Eng Phys 36(1):140–145
Hungr N, Long JA, Beix V, Troccaz J (2012) A realistic deformable prostate phantom for multimodal imaging and needle-insertion procedures. Med Phys 39(4):2031–2041
Betrouni N, Nevoux P, Leroux B, Colin P, Puech P, Mordon S (2013) An anatomically realistic and adaptable prostate phantom for laser thermotherapy treatment planning. Med Phys 40:022701
Bo LE, Leira HO, Tangen GA, Hofstad EF, Amundsen T, Lango T (2012) Accuracy of electromagnetic tracking with a prototype field generator in an interventional OR setting. Med Phys 39(1):399
Buyyounouski MK, Davis BJ, Prestidge BR, Shanahan TG, Stock RG, Grimm PD, Demanes DJ, Zaider M, Horwitz EM (2012) A survey of current clinical practice in permanent and temporary prostate brachytherapy: 2010 update. Brachytherapy 11(4):299
Seeberger R, Kane G, Hoffmann J, Eggers G (2012) Accuracy assessment for navigated maxillo-facial surgery using an electromagnetic tracking device. J Craniomaxillofac Surg 40(2):156–161
Lugez E, Pichora DR, Akl SG, Ellis RE (2013) Accuracy of electromagnetic tracking in an operating-room setting. In: Computer assisted radiology and surgery (CARS 2013). Heidelberg (abstract in International Journal of Computer Assisted Surgery and Radiology, vol. 8(1):147–148)
Lango T, Vijayan S, Rethy A, Vapenstad C, Solberg OV, Marvik R, Johnsen G, Hernes TN (2012) Navigated laparoscopic ultrasound in abdominal soft tissue surgery: technological overview and perspectives. Int J Comput Assist Radiol Surg 7(4):585–599
Lugez E, Pichora DR, Akl SG, Ellis RE (2013) Accuracy of electromagnetic tracking in an image-guided surgery suite. Bone Jt J Orthop Proc Suppl 95(Supp 28):25
Jain A, Kon R, Zhou Y, Fichtinger G (2005) C-arm calibration-is it really necessary? In: Medical image computing and computer-assisted intervention (MICCAI), pp 639–646
Wan G, Wei Z, Gardi L, Downey DB, Fenster A (2005) Brachytherapy needle deflection evaluation and correction. Med Phys 32:902
Acknowledgments
This work was supported in part through the Applied Cancer Research Unit program of Cancer Care Ontario with funds provided by the Ontario Ministry of Health and Long-Term Care. Gabor Fichtinger was funded as a Cancer Ontario Research Chair. Hossein Sadjadi was funded by the Natural Sciences and Engineering Research Council of Canada.
Conflict of interest
Hossein Sadjadi, Keyvan Hashtrudi-Zaad, and Gabor Fichtinger declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sadjadi, H., Hashtrudi-Zaad, K. & Fichtinger, G. Needle deflection estimation: prostate brachytherapy phantom experiments. Int J CARS 9, 921–929 (2014). https://doi.org/10.1007/s11548-014-0985-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-014-0985-0