Abstract
Purpose
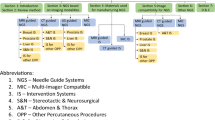
Percutaneous needle insertions are increasingly used for diagnosis and treatment of abdominal lesions. The challenging part of computed tomography (CT)-guided punctures is the transfer of the insertion trajectory planned in the CT image to the patient. Conventionally, this often results in several needle repositionings and control CT scans. To address this issue, several navigation systems for percutaneous needle insertions have been presented; however, none of them has thus far become widely accepted in clinical routine. Their benefit for the patient could not exceed the additional higher costs and the increased complexity in terms of bulky tracking systems and specialized markers for registration and tracking.
Methods
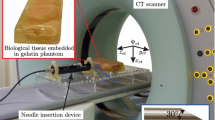
We present the first markerless and trackerless navigation concept for real-time patient localization and instrument guidance. It has specifically been designed to be integrated smoothly into the clinical workflow and does not require markers or an external tracking system. The main idea is the utilization of a range imaging device that allows for contactless and radiation-free acquisition of both range and color information used for patient localization and instrument guidance.
Results
A first feasibility study in phantom and porcine models yielded a median targeting accuracy of 6.9 and 19.4 mm, respectively.
Conclusions
Although system performance remains to be improved for clinical use, expected advances in camera technology as well as consideration of respiratory motion and automation of the individual steps will make this approach an interesting alternative for guiding percutaneous needle insertions.










Similar content being viewed by others
Notes
Note that the range data could as well be used to generate tracking information when post-processed with an instrument/object tracking algorithm (e.g., [39]). With the term tracking system, we refer to the widely applied definition where specialized hardware (cameras and tracking markers) are used for generating tracking information.
This porcine trial was approved by the Committee for Animal Care and Research of the Karlsruhe regional council (G-83/12).
The statistical power of these calculations (\(n = 10\)) may still not be sufficient to reliably detect significant differences.
Fig. 8 Targeting accuracies and registration error of the phantom study (“Phantom study’ section) with the markerless navigation system for PMD CamCube 3.0 and Microsoft Kinect for Xbox 360. The box plots show the targeting error divided into the overall error, the longitudinal error and the lateral error as well as the registration accuracy as the fiducial registration error (FRE) for all trials (\(N = 10\)) in mm (median, mininimum/maximum, upper/lower quartile)
Note that one trial was not considered in the error calculation due to an erroneous visualization of the implemented prototype which can easily be fixed in future versions.
References
Bale R, Widmann G, Schullian P, Haidu M, Pall G, Klaus A, Weiss H, Biebl M, Margreiter R (2011) Percutaneous stereotactic radiofrequency ablation of colorectal liver metastases. Eur Radiol 22(4):930–937
Banovac F, Cheng P, Campos-Nanez E, Kallakury B, Popa T, Wilson E, Abeledo H, Cleary K (2010) Radiofrequency ablation of lung tumors in swine assisted by a navigation device with preprocedural volumetric planning. J Vasc Interv Radiol 21(1):122–129
Bauer S, Seitel A, Hofmann H, Blum T, Wasza J, Balda M, Meinzer HP, Navab N, Hornegger J, Maier-Hein L (2013) Real-time range imaging in health care: a survey. In: Grzegorzek M, Theobalt C, Koch R, Kolb A (eds) Time-of-Flight and depth imaging. Sensors, algorithms, and applications, lecture notes in computer science, vol 8200. Springer, Berlin, pp 228–254
Besl PJ, McKay ND (1992) A method for registration of 3-D shapes. IEEE Trans Pattern Anal 14:239–256
Bolliger SA, Filograna L, Spendlove D, Thali MJ, Dirnhofer S, Ross S (2010) Postmortem imaging-guided biopsy as an adjuvant to minimally invasive autopsy with CT and postmortem angiography: a feasibility study. Am J Roentgenol 195(5):1051–1056
Boykov Y, Kolmogorov V (2004) An experimental comparison of Min-Cut/Max-Flow algorithms for energy minimization in vision. IEEE T Pattern Anal 26(9):1124–1137
Chetverikov D, Stepanov D, Krsek P (2005) Robust Euclidean alignment of 3D point sets: the trimmed iterative closest point algorithm. Image Vision Comput 23(3):299–309
Diotte B, Wang L, Weidert S, Thaller P, Euler E, Fallavollita P, Navab N (2012) Radiation-free drill guidance in interlocking of intramedullary nails. In: MICCAI 2012, part I, lecture notes in computer science, vol 7510, pp 18–25
dos Santos TR, Seitel A, Kilgus T, Suwelack S, Wekerle AL, Kenngott H, Speidel S, Schlemmer HP, Meinzer HP, Heimann T, Maier-Hein L (2014) Pose-independent surface matching for intra-operative soft-tissue marker-less registration. Med Image Anal 18(7):1101–1114
Fichtinger G, Deguet A, Fischer G, Iordachita I, Balogh E, Masamune K, Taylor RH, Fayad LM, de Oliveira M, Zinreich SJ (2005) Image overlay for CT-guided needle insertions. Comput Aided Surg 10(4):241–255
Fitzpatrick JM, West JB, Calvin R Maurer J (1998) Predicting error in rigid-body point-based registration. IEEE Trans Med Imaging 17:694–702
Foix S, Alenya G, Torras C (2011) Lock-in time-of-flight (ToF) cameras: a survey. IEEE Sensors J 11(9):1917–1926
Fuchs S, Hirzinger G (2008) Extrinsic and depth calibration of tof-cameras. In: IEEE conference on computer vision and pattern recognition
Grzegorzek M, Theobalt C, Koch R, Kolb A (eds) (2013) Time-of-Flight and depth imaging—sensors, algorithms, and applications. Springer, Berlin
Hollander M, Wol DA (1999) Nonparametric statistical methods. Wiley, New York
Horn BKP (1987) Closed-form solution of absolute orientation using unit quaternions. J Opt Soc Am 4:629
Hostettler A, Nicolau SA, Soler L, Rmond Y, Marescaux J (2008) A real-time predictive simulation of abdominal organ positions induced by free breathing. In: Biomedical simulation, lecture notes in computer science, vol 5104, pp 89–97
Khamene A, Wacker F, Vogt S, Azar F, Wendt M, Sauer F, Lewin J (2003) An augmented reality system for MRI-guided needle biopsies. Stud Health Technol Inf 94:151–157
Khan MF, Dogan S, Maataoui A, Gurung J, Schiemann M, Ackermann H, Wesarg S, Sakas G, Vogl TJ (2005) Accuracy of biopsy needle navigation using the Medarpa system-computed tomography reality superimposed on the site of intervention. Eur Radiol 15(11):2366–2374
Khati N, Gorodenker J, Hill M (2011) Ultrasound-guided biopsies of the abdomen. Ultrasound Q 27(4):255–268
Kilgus T, Heim E, Haase S, Prüfer S, Müller S. A.ller M, Seitel A, Fangerau M, Wiebe T, Iszatt J, Schlemmer HP, Hornegger J, Yen K, Maier-Hein L (2014) Mobile markerless augmented reality and its application in forensic medicine. Int J Comput Assist Radiol Surg (Epub ahead of print).doi:10.1007/s11548-014-1106-9
Kolb A, Barth E, Koch R, Larsen R (2009) Time-of-Flight sensors in computer graphics. In: Eurographics—state of the art reports, pp 119–134
Krücker J, Xu S, Venkatesan A, Locklin JK, Amalou H, Glossop N, Wood BJ (2011) Clinical utility of real-time fusion guidance for biopsy and ablation. J Vasc Interv Radiol 22(4):515–524
Maier-Hein L, Franz A, dos Santos T, Schmidt M, Fangerau M, Meinzer H, Fitzpatrick J (2012) Convergent iterative closest-point algorithm to accommodate anisotropic and inhomogenous localization error. IEEE Trans Pattern Anal 34(8):1520–1532
Maier-Hein L, Groch A, Bartoli A, Bodenstedt S, Boissonnat G, Chang PL, Clancy NT, Elson DS, Haase S, Heim E, Hornegger J, Jannin P, Kenngott H, Kilgus T, Muller-Stich B, Oladokun D, Rohl S, Dos Santos TR, Schlemmer HP, Seitel A, Speidel S, Wagner M, Stoyanov D (2014) Comparative validation of single-shot optical techniques for laparoscopic 3-D surface reconstruction. IEEE Trans Med Imaging 33(10):1913–1930
Maier-Hein L, Mountney P, Bartoli A, Elhawary H, Elson D, Groch A, Kolb A, Rodrigues M, Sorger J, Speidel S, Stoyanov D (2013) Optical techniques for 3D surface reconstruction in computer-assisted laparoscopic surgery. Med Image Anal 17(8):974–996
Maier-Hein L, Tekbas A, Seitel A, Pianka F, Müller SA, Satzl S, Schawo S, Radeleff B, Tetzlaff R, Franz AM, Müller-Stich BP, Wolf I, Kauczor HU, Schmied BM, Meinzer HP (2008) In vivo accuracy assessment of a needle-based navigation system for CT-guided radiofrequency ablation of the liver. Med Phys 35(12):5386–5396
Maleike D, Nolden M, Meinzer HP, Wolf I (2009) Interactive segmentation framework of the medical imaging interaction toolkit. Comput Meth Prog Biomed 96(1):72–83
Mersmann S, Seitel A, Erz M, Jähne B, Nickel F, Mieth M, Mehrabi A, Maier-Hein L (2013) Calibration of time-of-flight cameras for accurate intraoperative surface reconstruction. Med Phys 40(8):082701
Moser C, Becker J, Deli M, Busch M, Boehme M, Groenemeyer DHW (2013) A novel laser navigation system reduces radiation exposure and improves accuracy and workflow of CT-guided spinal interventions: a prospective, randomized, controlled, clinical trial in comparison to conventional freehand puncture. Eur J Radiol 82(4):627–632
Myronenko A, Song X (2010) Point set registration: coherent point drift. IEEE Trans Pattern Anal Mach Intell 32(12):2262–2275
Nagel M, Hoheisel M, Bill U, Klingenbeck-Regn K, Kalender WA, Petzold R (2008) Electromagnetic tracking system for minimal invasive interventions using a C-arm system with CT option: first clinical results. In: SPIE medical imaging 2008: visualization, image-guided procedures, and modeling
Nicolau S, Brenot J, Goffin L, Graebling P, Soler L, Marescaux J (2008) A structured light system to guide percutaneous punctures in interventional radiology. In: SPIE medical imaging: optical and digital image processing, p 700016
Nicolau SA, Pennec X, Soler L, Buy X, Gangi A, Ayache N, Marescaux J (2009) An augmented reality system for liver thermal ablation: design and evaluation on clinical cases. Med Image Anal 13(3):494–506
Nolden M, Zelzer S, Seitel A, Wald D, Müller M, Franz AM, Maleike D, Fangerau M, Baumhauer M, Maier-Hein L, Maier-Hein KH, Meinzer HP, Wolf I (2013) The medical imaging interaction toolkit: challenges and advances: 10 years of open-source development. Int J Comput Assist Radiol Surg 8(4):607–620
Oliveira-Santos T, Klaeser B, Weitzel T, Krause T, Nolte LP, Peterhans M, Weber S (2011) A navigation system for percutaneous needle interventions based on PET/CT images: design, workflow and error analysis of soft tissue and bone punctures. Comput Aided Surg 16(5):203–219
Otsu N (1979) A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern 9(1):62–66
Phee SJ, Yang K (2010) Interventional navigation systems for treatment of unresectable liver tumor. Med Biol Eng Comput 48(2):103–111
Prisacariu VA, Reid ID (2012) PWP3D: real-time segmentation and tracking of 3D objects. Int J Comput Vision 98(3):335–354
Seitel A, Engel M, Sommer CM, Radeleff BA, Essert-Villard C, Baegert C, Fangerau M, Fritzsche KH, Yung K, Meinzer HP, Maier-Hein L (2011) Computer-assisted trajectory planning for percutaneous needle insertions. Med Phys 38(6):3246–3259
Seitel A, Yung K, Mersmann S, Kilgus T, Groch A, Santos TRD, Franz AM, Nolden M, Meinzer HP, Maier-Hein L (2011) MITK-ToF range data within MITK. Int J Comput Assist Radiol Surg 7(1):87–96
Tomasi C, Manduchi R (1998) Bilateral filtering for gray and color images. In: Proceedings of the sixth international conference on computer vision (ICCV). IEEE Computer Society, Washington, DC, p 839
Wasza J, Bauer S, Hornegger J (2012) Real-time motion compensated patient positioning and non-rigid deformation estimation using 4-D shape priors. In: MICCAI 2012, Part II, lecture notes in computer science, vol 7511, pp 576–583
Wolf I, Vetter M, Wegner I, Böttger T, Nolden M, Schöbinger M, Hastenteufel M, Kunert T, Meinzer HP (2005) The medical imaging interaction toolkit. Med Image Anal 9(6):594–604
Wood BJ, Kruecker J, Abi-Jaoudeh N, Locklin JK, Levy E, Xu S, Solbiati L, Kapoor A, Amalou H, Venkatesan AM (2010) Navigation systems for ablation. J Vasc Interv Radiol 21(8 Suppl):S257–S263
Acknowledgments
This work was conducted within the settings of Research Training Group 1126: “Intelligent Surgery” funded by the German Research Foundation (DFG) and was partly supported by the DFG grant PD 15577. The authors would further like to thank Martina Jochim from the Department of Radiology at the German Cancer Research Center (DKFZ) for the assistance during the CT acquisitions, Adrian Winterstein for his help during the porcine trial and Christian Stock from the University Hospital Heidelberg for his statistical advise.
Conflict of interest
A. Seitel, N. Bellemann, M. Hafezi, A. Franz, M. Servatius, A. Saffari, T. Kilgus, H.-P. Schlemmer, A. Mehrabi, B. Radeleff and L. Maier-Hein declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Seitel, A., Bellemann, N., Hafezi, M. et al. Towards markerless navigation for percutaneous needle insertions. Int J CARS 11, 107–117 (2016). https://doi.org/10.1007/s11548-015-1156-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-015-1156-7