Abstract
Purpose
Mastoid cells as well as trabecula provide unique bone structures, which can serve as natural landmarks for registration. Preoperative imaging enables sufficient acquisition of these structures, but registration requires an intraoperative counterpart. Since versatile surgical interventions involve drilling into mastoid cells and trabecula, we propose a registration method based on endoscopy inside of these drill holes.
Methods
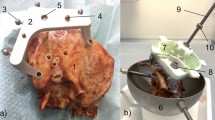
Recording of the surface of the inner drill hole yields bone-air patterns that provide intraoperative registration features. In this contribution, we discuss an approach that unrolls the drill hole surface into a two-dimensional image. Intraoperative endoscopic recordings are compared to simulated endoscopic views, which originate from preoperative data like computed tomography. Each simulated view corresponds to a different drill pose. The whole registration procedure and workflow is demonstrated, using high-resolution image data to simulate both preoperative and endoscopic image data.
Results
As the driving application is minimally invasive cochlear implantation, in which targets are close to the axis of the drill hole, Target Registration Error (TRE) was measured at points near the axis. TRE at increasing depths along the drill trajectory reveals increasing registration accuracy as more bone-air patterns become available as landmarks with the highest accuracy obtained at the center point. At the facial recess and the cochlea, TREs are (\(0.363\pm 0.169\)) mm and (\(0.553\pm 0.262\)) mm, respectively.
Conclusion
This contribution demonstrates a new method for registration via endoscopic acquisition of small features like trabecula or mastoid cells for image-guided procedures. It has the potential to revolutionize bone registration because it requires only a preoperative dataset and intraoperative endoscopic exploration. Endoscopic recordings of at least 20 mm length and isotropic voxel sizes of 0.2 mm or smaller of the preoperative image data are recommended.















Similar content being viewed by others
References
Bell B, Williamson T, Gerber N, Gavaghan K, Wimmer W, Kompis M, Weber S, Caversaccio M (2014) An image-guided robot system for direct cochlear access. Cochlear Implants Int 15(Suppl 1):S11–S13. doi:10.1179/1467010014Z.000000000192
Bergen T, Wittenberg TM (2014) Stitching and surface reconstruction from endoscopic image sequences: a review of applications and methods. IEEE J Biomed Heal Inform 2194(c):1–20. doi:10.1109/JBHI.2014.2384134
Bergmeier J, Daentzer D, Majdani O, Ortmaier T, Kahrs LA (2016) Image-to-physical registration based on endoscopy of a drill hole inside bone. In: CARS 2016—Computer Assisted Radiology Surgery Proceedings of the 30th international congress and exhibition Heidelberg, pp. 206–207. doi:10.1007/s11548-016-1412-5
Bergmeier J, Daentzer D, Noll C, Majdani O, Ortmaier T, Kahrs LA (2015)Towards endoscopic image-to-physical registration of mastoid cells and trabecula. In: Annual Conference of the German Society for Computer and Robot Assisted Surgery, pp. 43–48
Bergmeier J, Fast J, Ortmaier T, Kahrs LA (2017) Panorama imaging for image-to-physical registration of narrow drill holes inside spongy bones. In: Proceedings of SPIE, vol. 10135, pp. 1013507–1013507–12. doi:10.1117/12.2254417
Blumenfeld J, Carballido-Gamio J, Krug R, Blezek DJ, Hancu I, Majumdar S (2007) Automatic prospective registration of high-resolution trabecular bone images of the tibia. Ann Biomed Eng 35(11):1924–1931. doi:10.1007/s10439-007-9365-z
Deguchi D, Mori K, Suenaga Y, Hasegawa JI (2003) New image similarity measure for bronchoscope. MICCAI 2003 6th Int Conf Med Image Comput Comput Interv - 2878:399–406
Deligianni F, Chung A, Yang GZ (2003) pq-space based 2D/3D registration for endoscope tracking. In: MICCAI 2003 6th international conference of medical image computing and computer-assisted intervention pp. 311–318. doi:10.1007/978-3-540-39899-839
Díaz Díaz J, Riva M, Majdani O, Ortmaier T (2014) Normal distributions transform in multi-modal image registration of optical coherence tomography and computed tomography datasets. In: Proceedings of SPIE, pp. 90343L–90343L–7. doi:10.1117/12.2043623
Eggers G, Kress B, Mühling J (2008) Fully automated registration of intraoperative computed tomography image data for image-guided craniofacial surgery. J Oral Maxillofac Surg 66(8):1754–1760. doi:10.1016/j.joms.2007.12.019
Fitzpatrick JM, West JB, Maurer CR (1998) Predicting error in rigid-body point-based registration. IEEE Trans Med Imaging 17(5):694–702. doi:10.1109/42.736021
Gaa J, Kahrs LA, Müller S, Majdani O, Ortmaier T (2015) Cochlear shape description and analyzing via medial models. In: Proceedings of SPIE, 9413:941345–941345–6. doi:10.1117/12.2082033
Gerber N, Bell B, Gavaghan K, Weisstanner C, Caversaccio M, Weber S (2014) Surgical planning tool for robotically assisted hearing aid implantation. Int J Comput Assist Radiol Surg 9(1):11–20. doi:10.1007/s11548-013-0908-5
Igarashi T, Zenbutsu S, Yamanishi T, Naya Y (2008) Three-dimensional image processing system for the ureter and urethra using endoscopic video. J Endourol 22(8):1569–1572. doi:10.1089/end.2008.0150
Kahrs LA, Blachon GS, Balachandran R, Fitzpatrick JM, Labadie RF (2012) Measurement of distances between anatomical structures using a translating stage with mounted endoscope. In: Proceedings of SPIE, 8316:83160X–83160X–7. doi:10.1117/12.911464
Klenzner T, Ngan CC, Knapp FB, Knoop H, Kromeier J, Aschendorff A, Papastathopoulos E, Raczkowsky J, Wörn H, Schipper J (2009) New strategies for high precision surgery of the temporal bone using a robotic approach for cochlear implantation. Eur Arch Oto-Rhino-Laryngol 266(7):955–960. doi:10.1007/s00405-008-0825-3
Knoop H, Raczkowsky J, Wyslucha U, Fiegele T, Eggers G, Wörn H (2007) Integration of intraoperative imaging and surgical robotics to increase their acceptance. Int J Comput Assist Radiol Surg 1(5):243–251. doi:10.1007/s11548-006-0055-3
Labadie RF, Balachandran R, Noble JH, Blachon GS, Mitchell JE, Reda FA, Dawant BM, Fitzpatrick JM (2014) Minimally invasive image-guided cochlear implantation surgery: first report of clinical implementation. Laryngoscope 124(8):1915–1922. doi:10.1002/lary.24520
Lam SCB, Wald MJ, Rajapakse CS, Liu Y, Saha PK, Wehrli FW (2011) Performance of the MRI-based virtual bone biopsy in the distal radius: serial reproducibility and reliability of structural and mechanical parameters in women representative of osteoporosis study populations. Bone 49(4):895–903. doi:10.1016/j.bone.2011.07.010
Magland JF, Jones CE, Leonard MB, Wehrli FW (2009) Retrospective 3D registration of trabecular bone MR images for longitudinal studies. J Magn Reson Imaging 29(1):118–126. doi:10.1002/jmri.21551
Maier-Hein L, Mountney P, Bartoli A, Elhawary H, Elson D, Groch A, Kolb A, Rodrigues M, Sorger J, Speidel S, Stoyanov D (2013) Optical techniques for 3D surface reconstruction in computer-assisted laparoscopic surgery. Med Image Anal 17(8):974–996. doi:10.1016/j.media.2013.04.003
Majdani O, Rau TS, Baron S, Eilers H, Baier C, Heimann B, Ortmaier T, Bartling S, Lenarz T, Leinung M (2009) A robot-guided minimally invasive approach for cochlear implant surgery: preliminary results of a temporal bone study. Int J Comput Assist Radiol Surg 4(5):475–486. doi:10.1007/s11548-009-0360-8
Mattes D, Haynor DR, Vesselle H, Lewellen TK, Eubank W (2003) PET-CT image registration in the chest using free-form deformations. IEEE Trans Med Imaging 22(1):120–128. doi:10.1109/TMI.2003.809072
Nagaraja S, Skrinjar O, Guldberg RE (2011) Spatial correlations of trabecular bone microdamage with local stresses and strains using rigid image registration. J Biomech Eng 133(6):064,502. doi:10.1115/1.4004164
Quack VM, Kathrein S, Rath B, Tingart M, Lüring C (2012) Computer-assisted navigation in total knee arthroplasty: a review of literature. Biomed Tech 57(4):269–275. doi:10.1515/bmt-2011-0096
Rajapakse CS, Wald MJ, Magland J, Zhang XH, Liu XS, Guo XE, Wehrli FW (2009) Fast 3D registration of multimodality tibial images with significant structural mismatch. In: Proceedings of SPIE 7262:72620O–72620O–7. doi:10.1117/12.811753
Simpson AL, Burgner J, Glisson CL, Duke Herrell S, Ma B, Pheiffer TS, Webster RJ III, Miga MI (2013) Comparison study of intraoperative surface acquisition methods for surgical navigation. IEEE Trans Biomed Eng 60(4):1090–1099. doi:10.1109/TBME.2012.2215033
Sørensen MS, Dobrzeniecki AB, Larsen P, Frisch T, Sporring J, Darvann TA (2002) The visible ear: a digital image library of the temporal bone. ORL 64(6):378–381. doi:10.1159/000066089
Viola P, Wells W (1995) Alignment by maximization of mutual information. Proc IEEE Int Conf Comput Vis 24(2):16–23. doi:10.1109/ICCV.1995.466930
Wang H, Mirota D, Ishii M, Hager GD (2008) Robust motion estimation and structure recovery from endoscopic image sequences with an adaptive scale kernel consensus estimator. 26th IEEE Conference on Computer Vision and Pattern Recognition, CVPR. doi:10.1109/CVPR.2008.4587687
Williamson TM, Bell BJ, Gerber N, Salas L, Zysset P, Caversaccio M, Weber S (2013) Estimation of tool pose based on force-density correlation during robotic drilling. IEEE Trans Biomed Eng 60(4):969–976. doi:10.1109/TBME.2012.2235439
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the German Research Foundation (DFG) [KA 2975/4-1], [DA 1605/1-1], [MA 4038/10-1].
Conflict of interest
All authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Declaration of Helsinki and its later amendments or comparable ethical standards. Image data from the Visible Ear data set [28] have been used as cited.
Rights and permissions
About this article
Cite this article
Bergmeier, J., Fitzpatrick, J.M., Daentzer, D. et al. Workflow and simulation of image-to-physical registration of holes inside spongy bone. Int J CARS 12, 1425–1437 (2017). https://doi.org/10.1007/s11548-017-1594-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-017-1594-5