Abstract
Background
Hybrid operating rooms are used in different fields of surgery. In orthopedic surgery, the possibility of a 3D scan of difficult anatomical regions (spine, pelvis) showed promising results not only in navigated screw placement. The associated exposure to radiation raises questions regarding potential risks for the operating room personal and the patient. The present study focuses on scatter radiation during 3D scans in a hybrid operating room, the adjacent rooms, and methods to reduce radiation exposure.
Material and Methods
\(\hbox {RaySafe}^{\mathrm{TM}}\) i2 dosimeters were used to measure scatter radiation during 3D scans of different anatomical regions in different distances and heights in a hybrid operating room. The 3D scans were performed with a floor-based flat-panel robotic C-arm with 3D scan capability (Artis Zeego, Siemens; Germany). The 3D scans were performed using a human cadaver. The 3D scans were performed using a standard and a dose reduction protocol (DRP).
Results
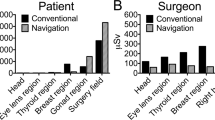
The highest scatter radiation was measured during 3D scans of the pelvis on the side of the surgical assistant (39.5 Sv in height of 1 m) compared to the side of the main surgeon (23 Sv in height of 1 m). Scatter radiation was less on the position of the scrub nurse (6.8 Sv in height of 1 m) and during 3D scans of the other anatomical regions. The radiation dosage was about 66% less with the DRP. Low values of scatter radiation were measured behind a radiation protection wall and with open doors in the adjacent rooms.
Conclusion
While performing a scan scatter radiation was measured everywhere in the operating room especially during 3D scans of the pelvic girdle. Therefore, settings with lower dosage should be used whenever possible. Personnel should stand behind a radiation safety wall or leave the operating room and close the doors. For this study, six behavioral rules to avoid radiation in a hybrid operating room were established.









Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Change history
15 June 2018
The original version of this article unfortunately contained a mistake. In abstract, results section should read.
17 February 2022
A Correction to this paper has been published: https://doi.org/10.1007/s11548-022-02569-4
References
Tsagakis K, Konorza T, Dohle DS, Kottenberg E, Buck T, Thielmann M, Erbel R, Jakob H (2013) Hybrid operating room concept for combined diagnostics, intervention and surgery in acute type A dissection. Eur J Cardiothorac Surg Off J Eur Assoc Cardiothorac Surg 43(2):397–404
Hlavac M, Konig R, Halatsch M, Wirtz CR (2012) Intraoperative magnetic resonance imaging. Fifteen years’ experience in the neurosurgical hybrid operating suite. Der Unfallchirurg 115(2):121–4
Fandino J, Taussky P, Marbacher S, Muroi C, Diepers M, Fathi AR, Remonda L (2013) The concept of a hybrid operating room: applications in cerebrovascular surgery. Acta Leurochirurgica Suppl 115:113–7
Terra RM, Andrade JR, Mariani AW, Garcia RG, Succi JE, Soares A, Zimmer PM (2016) Applications for a hybrid operating room in thoracic surgery: from multidisciplinary procedures to—image-guided video-assisted thoracoscopic surgery. J Bras Pneumol 42(5):387–90
Varu VN, Greenberg JI, Lee JT (2013) Improved efficiency and safety for EVAR with utilization of a hybrid room. Eur J Casc Endovasc Surg Off J Eur Soc Vasc Surg 46(6):675–9
Steinbauer M, Katsargyris A, Greindl M, Topel I, Verhoeven E (2013) Hybrid operation theatre in vascular surgery. Options and perspectives. Der Chirurg; Zeitschrift fur alle Gebiete der operativen Medizen 84(12):1030–5
Richter PH, Gebhard F, Dehner C, Scola A (2016) Accuracy of computer-assisted iliosacral screw placement using a hybrid operating room. Injury 47(2):402–7
Kendrick DE, Miller CP, Moorehead PA, Kim AH, Baele HR, Wong VL, Jordan DW, Kashyap VS (2016) Comparative occupational radiation exposure between fixed and mobile imaging systems. J Vasc Surg 63(1):190–7
van den Haak RF, Hamans BC, Zuurmond K, Verhoeven BA, Koning OH (2015) Significant radiation dose reduction in the hybrid operating room using a novel X-ray imaging technology. Eur J Vasc Endovasc Surg Off J Eur Soc Vasc Surg 50(4):480–6
Kesavachandran CN, Haamann F, Nienhaus A (2012) Radiation exposure of eyes, thyroid gland and hands in orthopaedic staff: a systematic review. Eur J Med Res 17:28
Pokrywka M, Byers K (2013) Traffic in the operating room: a review of factors influencing air flow and surgical wound contamination. Infect Disord Drug Targets 13(3):156–61
Darouiche RO, Green DM, Harrington MA, Ehni BL, Kougias P, Bechara CF, O’Connor DP (2017) Association of airborne microorganisms in the operating room with implant infections: a randomized controlled trial. Infect Control Hosp Epidemiol 38(1):3–10
Cristina ML, Sartini M, Schinca E, Ottria G, Spagnolo AM (2016) Operating room environment and surgical site infections in arthroplasty procedures. J Prev Med Hyg 57(3):E142–E8
Knobben BA, van Horn JR, van der Mei HC, Busscher HJ (2006) Evaluation of measures to decrease intra-operative bacterial contamination in orthopaedic implant surgery. J Hosp Infect 62(2):174–80
Andersson AE, Bergh I, Karlsson J, Eriksson BI, Nilsson K (2012) Traffic flow in the operating room: an explorative and descriptive study on air quality during orthopedic trauma implant surgery. Am J Infect Control 40(8):750–5
Romanova K, Vassileva J, Alyakov M (2015) Radiation exposure to the eye lens of orthopaedic surgeons during various orthopaedic procedures. Radiat Prot Dosim 165(1–4):310–3
Schulz B, Heidenreich R, Heidenreich M, Eichler K, Thalhammer A, Naeem NN, Vogl TJ, Zangos S (2012) Radiation exposure to operating staff during rotational flat-panel angiography and C-arm cone beam computed tomography (CT) applications. Eur J Radiol 81(12):4138–42
Hendee WR, Edwards FM (1986) ALARA and an integrated approach to radiation protection. Semin Nucl Med 16(2):142–50
Bahari S, Morris S, Broe D, Taylor C, Lenehan B, McElwain J (2006) Radiation exposure of the hands and thyroid gland during percutaneous wiring of wrist and hand procedures. Acta Orthop Belg 72(2):194–8
Srinivasan D, Than KD, Wang AC, La Marca F, Wang PI, Schermerhorn TC, Park P (2014) Radiation safety and spine surgery: systematic review of exposure limits and methods to minimize radiation exposure. World Neurosurg 82(6):1337–43
Kaplan DJ, Patel JN, Liporace FA, Yoon RS (2016) Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient Saf Surg. 10:27
Kraus M, Fischer E, Gebhard F, Richter PH (2016) Image quality and effective dose of a robotic flat panel 3D C-arm vs computed tomography. Int J Med Robot 12(4):743–50
Racadio J, Nachabe R, Carelsen B, Racadio J, Hilvert N, Johnson N, Kukreja K, Patel M (2014) Effect of real-time radiation dose feedback on pediatric interventional radiology staff radiation exposure. J Vasc Interv Radiol: JVIR 25(1):119–26
Baumann F, Katzen BT, Carelsen B, Diehm N, Benenati JF, Pena CS (2015) The effect of realtime monitoring on dose exposure to staff within an interventional radiology setting. Cardiovasc Interv Radiol 38(5):1105–11
Muller MC, Welle K, Strauss A, Naehle PC, Pennekamp PH, Weber O, Burger C (2014) Real-time dosimetry reduces radiation exposure of orthopaedic surgeons. Orthop Traumatol Surg Res: OTSR. 100(8):947–51
Funding
This work was partially funded by the AO Trauma Foundation through a Grant S-13-128K.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest. No company had influence in the collection of data or contributed to or had influence on the conception, design, analysis and writing of the study. No further funding was received
Ethical approval
The study was approved by the local and has been performed in accordance with the ethical standards in the 1964 Declaration of Helsinki
Rights and permissions
About this article
Cite this article
Schuetze, K., Kraus, M., Eickhoff, A. et al. Radiation exposure for intraoperative 3D scans in a hybrid operating room: how to reduce radiation exposure for the surgical team. Int J CARS 13, 1291–1300 (2018). https://doi.org/10.1007/s11548-018-1747-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1747-1