Abstract
Purpose
Flexible needle has the potential to accurately navigate to a treatment region in the least invasive manner. We propose a new planning method using Markov decision processes (MDPs) for flexible needle navigation that can perform robust path planning and steering under the circumstance of complex tissue–needle interactions.
Methods
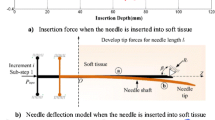
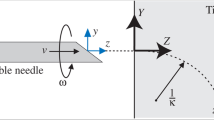
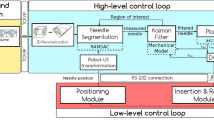
This method enhances the robustness of flexible needle steering from three different perspectives. First, the method considers the problem caused by soft tissue deformation. The method then resolves the common needle penetration failure caused by patterns of targets, while the last solution addresses the uncertainty issues in flexible needle motion due to complex and unpredictable tissue–needle interaction.
Results
Computer simulation and phantom experimental results show that the proposed method can perform robust planning and generate a secure control policy for flexible needle steering. Compared with a traditional method using MDPs, the proposed method achieves higher accuracy and probability of success in avoiding obstacles under complicated and uncertain tissue–needle interactions. Future work will involve experiment with biological tissue in vivo.
Conclusion
The proposed robust path planning method can securely steer flexible needle within soft phantom tissues and achieve high adaptability in computer simulation.














Similar content being viewed by others
References
Fuchs KH (2002) Minimally invasive surgery. Endoscopy 34(02):154–159
Rosen M, Ponsky J (2001) Minimally invasive surgery. Endoscopy 33(04):358–366
Abolhassani N, Patel R, Moallem M (2007) Needle insertion into soft tissue: a survey. Med Eng Phys 29(4):413–431
Doi K (2007) Computer-aided diagnosis in medical imaging: historical review, current status and future potential. Comput Med Imaging Graph 31(4):198–211
Nath S, Chen Z, Yue N, Trumpore S, Peschel R (2000) Dosimetric effects of needle divergence in prostate seed implant using 125i and 103pd radioactive seeds. Med Phys 27(5):1058–1066
Carr JJ, Hemler PF, Halford PW, Freimanis RI, Choplin RH, Chen MYM (2001) Stereotactic localization of breast lesions: how it works and methods to improve accuracy. Radiographics 21(2):463–473
Taschereau R, Pouliot J, Roy J, Tremblay D (2000) Seed misplacement and stabilizing needles in transperineal permanent prostate implants. Radiother Oncol 55(1):59–63
Narayana V, Roberson PL, Winfield RJ, Kessler ML, McLaughlin PW (1996) Optimal placement of radioisotopes for permanent prostate implants. Radiology 199(2):457–460
Alterovitz R, Branicky M, Goldberg K (2008) Motion planning under uncertainty for image-guided medical needle steering. Int J Robot Res 27(11–12):1361–1374
Donaldson MS, Corrigan JM, Kohn LT (2000) To err is human: building a safer health system, vol 6. National Academies Press, Washington
Robert J, Webster III, Kim JS, Cowan NJ, Chirikjian GS, Okamura AM (2006) Nonholonomic modeling of needle steering. Int J Robot Res 25(5–6):509–525
Webster RJ, Memisevic J, Okamura AM (2005) Design considerations for robotic needle steering. In: Proceedings of the 2005 IEEE international conference on robotics and automation, ICRA 2005. IEEE, pp 3588–3594
Leong F, Huang W-H, Chui C-K (2013) Modeling and analysis of coagulated liver tissue and its interaction with a scalpel blade. Med Biol Eng Comput 51(6):687–695
Fu YB, Chui CK (2014) Modelling and simulation of porcine liver tissue indentation using finite element method and uniaxial stress–strain data. J Biomech 47(10):2430–2435
Fu YB, Chui CK, Teo CL (2013) Liver tissue characterization from uniaxial stress-strain data using probabilistic and inverse finite element methods. J Mech Behav Biomed Mater 20:105–112
O’Reilly MS, Boehm T, Shing Y, Fukai N, Vasios G, Lane WS, Flynn E, Birkhead JR, Olsen BR, Folkman J (1997) Endostatin: an endogenous inhibitor of angiogenesis and tumor growth. Cell 88(2):277–285
Abayazid M, Vrooijink GJV, Patil S, Alterovitz R, Misra S (2014) Experimental evaluation of ultrasound-guided 3d needle steering in biological tissue. Int J Comput Assist Radiol Surg 9(6):931–939
Vrooijink JG, Abayazid M, Patil S, Alterovitz R, Misra S (2014) Needle path planning and steering in a three-dimensional non-static environment using two-dimensional ultrasound images. Int J Robot Res 33(10):1361–1374
Patil S, Burgner J, Webster RJ, Alterovitz R (2014) Needle steering in 3-d via rapid replanning. IEEE Trans Robot 30(4):853–864
Alterovitz R, Lim A, Goldberg K, Chirikjian GS, Okamura AM (2005) Steering flexible needles under Markov motion uncertainty. In: 2005 IEEE/RSJ international conference on intelligent robots and systems, (IROS 2005). IEEE, pp 1570–1575
Alterovitz R, Siméon T, Goldberg KY (2007) The stochastic motion roadmap: a sampling framework for planning with Markov motion uncertainty. In: Robotics: science and systems, vol 3, pp 233–241
Pengqian Y, Huan X (2016) Distributionally robust counterpart in Markov decision processes. IEEE Trans Autom Control 61(9):2538–2543
DiMaio S, Salcudean SE (2003) Needle insertion modeling and simulation. IEEE Trans Robot Autom 19(5):864–875
DiMaio PS, Salcudean SE (2005) Needle steering and motion planning in soft tissues. IEEE Trans Biomed Eng 52(6):965–974
Glozman D, Shoham M (2006) Flexible needle steering for percutaneous therapies. Computer Aided Surg 11(4):194–201
Kallem V, Cowan NJ (2009) Image guidance of flexible tip-steerable needles. IEEE Trans Robot 25(1):191–196
Shahriari N, Roesthuis RJ, van de Berg NJ, van den Dobbelsteen JJ, Misra S (2016) Steering an actuated-tip needle in biological tissue: fusing fbg-sensor data and ultrasound images. In: 2016 IEEE international conference on robotics and automation (ICRA). IEEE, pp 4443–4449
Suetens P (2017) Fundamentals of medical imaging. Cambridge University Press, Cambridge
Thie PR (1983) Markov decision processes. Comap, Incorporated, Bedford
Bertsekas DP, Bertsekas DP, Bertsekas DP, Bertsekas DP (1995) Dynamic programming and optimal control, vol 1. Athena Scientific, Belmont
Mostafa A, Fouad A, Elfattah MA, Hassanien AE, Hefny H, Zhu SY, Schaefer G (2015) Ct liver segmentation using artificial bee colony optimisation. Proc Comput Sci 60:1622–1630
Norajitra T, Meinzer H-P, Maier-Hein KH (2015) 3d statistical shape models incorporating 3d random forest regression voting for robust ct liver segmentation. In: Proceedings of SPIE, vol 9414, p 941406
Duan B, Wen R, Chng C-B, Wang W, Liu P, Qin J, Peneyra JL, Chang Stephen K-Y, Heng P-A, Chui C-K (2015) Image-guided robotic system for radiofrequency ablation of large liver tumor with single incision. In: 2015 12th international conference on ubiquitous robots and ambient intelligence (URAI). IEEE, pp 284–289
Yang L, Wen R, Qin J, Chui C-K, Lim K-B, Chang SK-Y (2010) A robotic system for overlapping radiofrequency ablation in large tumor treatment. IEEE/ASME Trans Mechatron 15(6):887–897
Liu Y, Kerdok AE, Howe RD (2004) A nonlinear finite element model of soft tissue indentation. Lect Notes Comput Sci 3078:67–76
Varadhan G, Manocha D (2006) Accurate Minkowski sum approximation of polyhedral models. Graph Models 68(4):343–355
van de Berg NJ, van Gerwen DJ, Dankelman J, van den Dobbelsteen JJ (2015) Design choices in needle steeringa review. IEEE/ASME Trans Mechatron 20(5):2172–2183
Tan X, Chng C-B, Duan B, Ho Y, Wen R, Chen X, Lim K-B, Chui C-K (2016) Design and implementation of a patient-specific cognitive engine for robotic needle insertion. In: 2016 IEEE international conference on systems, man, and cybernetics (SMC). IEEE, pp 000560–000565
Tan X, Chng C-B, Duan B, Ho Y, Wen R, Chen X, Lim K-B, Chui C-K (2017) Cognitive engine for robot-assisted radio-frequency ablation system. Acta Polytech Hung 14(1):129–145
Funding
The research and development of the prototype image-guide radio-frequency ablation surgical system was supported in parts by research grants from Singapore Agency of Science and Technology (A*Star) and Ministry of Education, Singapore, respectively.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Human participants
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tan, X., Yu, P., Lim, KB. et al. Robust path planning for flexible needle insertion using Markov decision processes. Int J CARS 13, 1439–1451 (2018). https://doi.org/10.1007/s11548-018-1783-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1783-x