Abstract
Purpose
Ventricular septal defects (VSD) are congenital heart malformations and, in severe cases, they require complex interventions under echocardiography guidance. Heart phantoms can be helpful to train and to understand the complex hemodynamics of VSD. The goal of this study was to characterize the best blood mimicking fluids in such heart phantoms for modelling the hemodynamics of VSD patients using echocardiography.
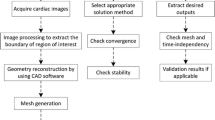
Methods
Four fluid compositions were considered. Distilled water was used as a baseline, while the other three fluids were developed based on physical properties of human blood, such as the viscosity and the refractive index. Three bi-ventricular heart phantoms of three different pediatric patients with complex VSD were designed from preoperative CT imaging. Custom molds were printed in 3-D and the anatomical structure was casted in polyvinyl alcohol cryogel. The VSD in each heart phantom were observed using echocardiography and color Doppler imaging was used for the hemodynamic study.
Results
Heart phantoms with blood mimicking fluids of 30% glycerol and 27% glycerol, 10% sodium iodide were found to be anatomically realistic under echocardiography imaging. Hemodynamic parameters such as the pressure gradient and the volume of the shunt were characterized using color Doppler imaging.
Conclusion
Proper composition of blood mimicking fluids are important for improving the realism in echocardiographic heart phantoms and they contribute to better understand the complex hemodynamic of VSD under echocardiography.





Similar content being viewed by others
Data availability
The clinical datasets cannot be publicly released. The material used in this study is commercially available.
References
Congenital anomalies in Canada 2013: a perinatal health surveillance report by the Public Health Agency of Canada's Canadian Perinatal Surveillance System, HPCDPC, Health Canada
Dakkak W, Oliver TI (2021) Ventricular septal defect. StatPearls Publishing
Antigoni D, English K (2018) Echocardiographic assessment of left to right shunts: atrial septal defect, ventricular septal defect, atrioventricular septal defect, patent arterial duct. Echo Res Practice 5(1):R1-16
Kwartowitz DM, Mefleh FN, Baker GH (2017) Toward computer-assisted image-guided congenital heart defect repair: an initial phantom analysis. Int J Comput Assist Radiol Surg 12(10):1839–1844
Engelhardt S, Sauerzapf S, Preim B, Karck M, Wolf I, De Simone R (2019) Flexible and comprehensive patient-specific mitral valve silicone models with chordae tendineae made from 3D-printable molds. Int J Comput Assist Radiol Surg 14(7):1177–1186
Nisar H, Moore J, Piazza R, Maneas E, Chen ECS, Peters TM (2020) A simple, realistic walled phantom for intravascular and intracardiac applications. Int J Comput Assist Radiol Surg 15(9):1513–1523
Awori J, Friedman SD, Chan T, Howard C, Seslar S, Soriano BD, Buddhe S (2021) 3D models improve understanding of congenital heart disease. 3D Print Med 7(1):26
Yoo SJ, Thabit O, Kim EK, Ide H, Yim D, Dragulescu A, Seed M, Grosse-Wortmann L, Arsdell G (2015) 3D Printing in medicine of congenital heart diseases. M3D Print Med 2(1):3
Gómez-Ciriza G, Gómez-Cía T, Rivas-González JA, Velasco Forte MN, Valverde I (2021) Affordable three-dimensional printed heart models. Front Cardiovasc Med 4(8):642011
Yamada T, Osaka M, Uchimuro T, Yoon R, Morikawa T, Sugi-moto M, Suda H, Shimizu H (2017) Three-dimensional printing of life-like models for simulation and training of minimally invasive cardiac surgery. Innovations 12(6):459–465
Morais P, Tavares JMR, Queiros S et al (2017) Development of a patient-specific atrial phantom model for planning and training of inter-atrial interventions. Med Phys 44(11):5638–5649
Tibamoso-Pedraza G, Navarro I, Dion P, Raboisson MJ, Lapierre C, Miró J, Ratté S, Duong L (2021) Design of heart phantoms for ultrasound imaging of ventricular septal defects. Int J Comput Assist Radiol Surg 17:177
Bazan O, Ortiz JP (2016) Experimental validation of a cardiac simulator for in vitro evaluation of prosthetic heart valves. Braz J Cardiovasc Surg 31(2):151–157
Oglat AA, Matjafri MZ, Suardi N, Oqlat MA, Abdelrahman MA, Oqlat AA, Farhat OF, Alkhateb BN, Abdalrheem R, Ahmad MS, Abujazar MYM (2018) Chemical items used for preparing tissue-mimicking material of wall-less flow phantom for Doppler ultrasound imaging. J Med Ultrasound 26(3):123–127
Ramnarine KV, Nassiri DK, Hoskins PR, Lubbers J (1998) Validation of a new blood- mimicking fluid for use in Doppler flow test objects. Ultrasound Med Biol 24(3):451–459
Youssif M, Holdsworth DW, Poepping TL (2011) A blood-mimicking fluid for particle image velocimetry with silicone vascular models. Exp Fluids 50(3):769–774
Simpson J, Lopez L, Acar P, Friedberg MK, Khoo NS, Ko HH, Marek J, Marx G, McGhie JS, Meijboom F, Roberson D, Van den Bosch A, Miller O, Shirali G (2017) Three-dimensional echocardiography in congenital heart disease: an expert consensus document from the European Association of Cardiovascular Imaging and the American Society of Echocardiography. J Am Soc Echocardiogr 30(1):1–27
Hadeed K, Hascoet S, Amadieu R, Karsenty C, Cuttone F, Leobon B, Dulac Y, Acar P (2016) Assessment of ventricular septal defect size and morphology by three-dimensional transthoracic echocardiography. J Am Soc Echocardiogr 29(8):777–785
Tortora GJ, Derrickson, BH (2015) Principes d’anatomie et de physiologie
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Ethics approval
Institutional review board approval from CHU Sainte-Justine was obtained for this retrospective study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Amouri, S., Tibamoso-Pedraza, G., Navarro-Castellanos, I. et al. Characterization of blood-mimicking fluids for echocardiography imaging of ventricular septal defects. Int J CARS 17, 1601–1609 (2022). https://doi.org/10.1007/s11548-022-02686-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-022-02686-0