Abstract
Purpose
Surgical devices or systems typically operate in a stand-alone manner, making it difficult to perform integration analysis of both intraoperative anatomical and functional information. To address this issue, the intraoperative information integration system OPeLiNK® was developed. The objective of this study is to generate information for decision making using surgical navigation and intraoperative monitoring information accumulated in the OPeLiNK® database and to analyze its utility.
Methods
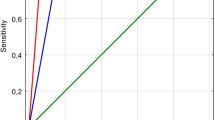
We accumulated intraoperative information from 27 brain tumor patients who underwent resection surgery. First, the risk rank for postoperative paralysis was set according to the attenuation rate and amplitude width of the motor evoked potential (MEP). Then, the MEP and navigation log data were combined and plotted on an intraoperative magnetic resonance image of the individual brain. Finally, statistical parametric mapping (SPM) transformation was performed to generate a standard brain risk map of postoperative paralysis. Additionally, we determined the anatomical high-risk areas using atlases and analyzed the relationship with each set risk rank.
Results
The average distance between the navigation log corresponding to each MEP risk rank and the anatomical high-risk area differed significantly between the with postoperatively paralyzed and without postoperatively paralyzed groups, except for “safe.” Furthermore, no excessive deformation was observed resulting from SPM conversion to create the standard brain risk map. There were cases in which no postoperative paralysis occurred even when MEP decreased intraoperatively, and vice versa.
Conclusion
The time synchronization reliability of the study data is very high. Therefore, our created risk map can be reported as being functional at indicating the risk areas. Our results suggest that the statistical risks of postoperative complications can be presented for each area where brain surgery is to be performed. In the future, it will be possible to provide surgical navigation with intraoperative support that reflects the risk maps created.






Similar content being viewed by others
References
Ciric I, Ammirati M, Vick N, Mikhael M (1987) Supratentorial gliomas: surgical considerations and immediate postoperative results; gross total resection versus partial resection. Neurosurgery 21:21–26. https://doi.org/10.1227/00006123-198707000-00005
Berger MS, Rostomily RCT (1997) Low grade gliomas: functional mapping resection strategies, extent of resection, and outcome. J Neurooncol 34:85–101. https://doi.org/10.1023/a:1005715405413
Mikuni N, Okada T, Enatsu R, Miki Y, Hanakawa T, Urayama S, Kikuta K, Takahashi JA, Nozaki K, Fukuyama H, Hashimoto N (2007) Clinical impact of integrated functional neuronavigation and subcortical electrical stimulation to preserve motor function during resection of brain tumors. J Neurosurg 106:593–598. https://doi.org/10.3171/jns.2007.106.4.593
Muragaki Y, Iseki H, Maruyama T, Tanaka M, Shinohara C, Suzuki T, Yoshimittsu K, Ikuta S, Hayashi M, Chernov M, Hori T, Okada Y (2011) Information-guided surgical management of gliomas using low-field-strength intraoperative MRI. Acta Neurochir Suppl 109:67–72. https://doi.org/10.1007/978-3-211-99651-5_11
Saito T, Muragaki Y, Miura I, Tamura M, Maruyama T, Nitta M, Kurisu K, Iseki H, Okada Y (2014) Functional plasticity of language confirmed with intraoperative electrical stimulations and updated neuronavigation: case report of low-grade glioma of the left inferior frontal gyrus. Neurol Med Chir (Tokyo) 54:587–659. https://doi.org/10.2176/nmc.cr.2013-0248
Sicking J, Voß KM, Spille DC, Schipmann S, Holling M, Paulus W, Hess K, Steinbicker AU, Stummer W, Grauer O, Wölfer J, Brokinkel B (2018) The evolution of cranial meningioma surgery—a single-center 25-year experience. Acta Neurochir (Wien) 160:1801–1812. https://doi.org/10.1007/s00701-018-3617-6
Kombos T, Suess O, Ciklatekerlio Ö, Brock M (2001) Monitoring of intraoperative motor evoked potentials to increase the safety of surgery in and around the motor cortex. J Neurosurg 95:608–614. https://doi.org/10.3171/jns.2001.95.4.0608
Taniguchi M, Cedzich C, Schramm J (1993) Modification of cortical stimulation for motor evoked potentials under general anesthesia: a technical description. Neurosurgery 32:219–266. https://doi.org/10.1227/00006123-199302000-00011
Langeloo DD, Lelivelt A, Louis Journée H, Slappendel R, de Kleuver M (2003) Transcranial electrical motor-evoked potential monitoring during surgery for spinal deformity: a study of 145 patients. Spine 28:1043–1050. https://doi.org/10.1097/01.BRS.0000061995.75709.78
Kamada K, Todo T, Ota T, Ino K, Masutani Y, Aoki S, Takeuchi F, Kawai K, Saito N (2009) The motor-evoked potential threshold evaluated by tractography and electrical stimulation. J Neurosurg 111(4):785–795. https://doi.org/10.3171/2008.9.JNS08414
Maesawa S, Fujii M, Nakahara N, Watanabe T, Wakabayashi T, Yoshida J (2010) Intraoperative tractography and motor evoked potential (MEP) monitoring in surgery for gliomas around the corticospinal trace. World Neurosurg 74:153–161. https://doi.org/10.1016/j.wneu.2010.03.022
Moiyadi A, Velayutham P, Shetty P, Seidel K, Janu A, Madhugiri V, Singh VK, Patil A, John R (2008) Combined motor evoked potential monitoring and subcortical dynamic mapping in motor eloquent tumors allows safer and extended resections. World Neurosurg 120:e259–e268. https://doi.org/10.1016/j.wneu.2018.08.046
Ozawa N, Muragaki Y, Nakamura R, Iseki H (2009) Identification of the pyramidal tract by neuronavigation based on intraoperative diffusion-weighted imaging combined with subcortical stimulation. Stereotract Funct Neurosurg 87:18–24. https://doi.org/10.1159/000177624
Okamoto J, Masamune K, Iseki H, Muragaki Y (2017) Development concepts of a Smart Cyber Operating Theater (SCOT) using ORiN technology. Biomed Tech (Berl) 63:31–37. https://doi.org/10.1515/bmt-2017-0006
Tokuda J, Fischer GS, Papademetris X, Yaniv Z, Ibanez L, Cheng P, Liu H, Blevins J, Arata J, Golby AJ, Kapur T, Pieper S, Burdette EC, Fichtinger G, Tempany CM, Hata N (2009) OpenIGTLink: an open network protocol for image-guided therapy environment. Int J Med Robot 5:423–434. https://doi.org/10.1002/rcs.274
Fujiki M, Furukawa Y, Kamida T, Ana M, Inoue R, Abe T, Kobayashi H (2006) Intraoperative corticomuscular motor evoked potentials for evaluation of motor function: a comparison with corticospinal D and I waves. J Neurosurg 104:185–192. https://doi.org/10.1002/rcs.274
Zhou HH, Kelly PJ (2001) Transcranial electrical motor evoked potential monitoring for brain tumor resection. Neurosurg 48:1075–1081. https://doi.org/10.1097/00006123-200105000-00021
Saito T, Tamura M, Muragaki Y, Maruyama T, Kubota Y, Fukuchi S, Nitta M, Chernov M, Okamoto S, Sugiyama K, Kurisu K, Sakai KL, Okada Y, Iseki H (2014) Intraoperative cortico-cortical evoked potentials for the evaluation of language function during brain tumor resection: initial experience with 13 cases. J Neurosurg 121:827–838. https://doi.org/10.3171/2014.4.JNS131195
Ashburner J, Friston KJ (1999) Nonlinear spatial normalization using basis functions. Hum Brain Mapp 7:254–266. https://doi.org/10.1002/(SICI)1097-0193(1999)7:4%3c254::AID-HBM4%3e3.0.CO;2-G
Desikan RS, Ségonne F, Fischl B, Quinn BT, Dickerson BC, Blacker D, Buckner RL, Dale AM, Maguire RP, Hyman BT, Albert MS, Killiany RJ (2006) An automated labeling system for subdividing the human cerebral cortex on MRI scans into gyral based regions of interest. Neuroimage 31:968–980. https://doi.org/10.1016/j.neuroimage.2006.01.021
Mori S, Oishi K, Jiang H, Jiang L, Li X, Akhter K, Hua K, Faria AV, Mahmood A, Woods R, Toga AW, Pike GB, Neto PR, Evans A, Zhang J, Huang H, Miller MI, van Zijl P, Mazziotta J (2008) Stereotaxic white matter atlas based on diffusion tensor imaging in an ICBM template. Neuroimage 40:570–582. https://doi.org/10.1016/j.neuroimage.2007.12.035
Krieg SM, Shiban E, Droese D, Gempt J, Buchmann N, Pape H, Ryang Y, Meyer B, Ringel F (2012) Predictive value and safety of intraoperative neurophysiological monitoring with motor evoked potentials in glioma surgery. Neurosurgery 70:1060–1071. https://doi.org/10.1227/NEU.0b013e31823f5ade
Suess O, Suess S, Brock M, Kombos T (2006) Intraoperative electrocortical stimulation of Brodman area 4: a 10-year analysis of 255 cases. Head Face Med 2:20. https://doi.org/10.1186/1746-160X-2-20
Kombos T, Picht T, Derdilopoulos A, Suess O (2009) Impact of intraoperative neurophysiological monitoring on surgery of high-grade gliomas. J Clin Neurophysiol 26:422–425. https://doi.org/10.1007/s00701-018-3732-4
Yamamoto T, Katayama Y, Nagaoka T, Kobayashi K, Fukaya C (2004) Intraoperative monitoring of the corticospinal motor evoked potential (D-wave) clinical index for postoperative motor function and functional recovery. Neurol Med Chir (Tokyo) 44:170–182. https://doi.org/10.2176/nmc.44.170
Acknowledgements
This research was partly supported by a Grant-in-Aid for Research Activity Start-up from JSPS KAKENHI, Grant Number 20K23349.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
T. Yamaguchi, A. Kuwano, T. Saito, K. Masamune and Y. Muragaki declare that they have no conflicts of interest. T. Koyama is an employee of DENSO Corporation. J. Okamoto is Vice President and Chief Operations Officer of SONIRE Therapeutics Inc. S. Suzuki is Chief Technical Officer of OPExPARK Inc. H. Okuda is Executive Vice President and Founder of OPExPARK Inc. and an employee of DENSO Corporation.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Yamaguchi, T., Kuwano, A., Koyama, T. et al. Construction of brain area risk map for decision making using surgical navigation and motor evoked potential monitoring information. Int J CARS 18, 269–278 (2023). https://doi.org/10.1007/s11548-022-02752-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-022-02752-7