Abstract
Purpose
Preprocedural planning is a key step in radiofrequency ablation (RFA) treatment for liver tumors, which is a complex task with multiple constraints and relies heavily on the personal experience of interventional radiologists, and existing optimization-based automatic RFA planning methods are very time-consuming. In this paper, we aim to develop a heuristic RFA planning method to rapidly and automatically make a clinically acceptable RFA plan.
Methods
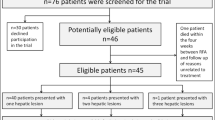
First, the insertion direction is heuristically initialized based on tumor long axis. Then, the 3D RFA planning is divided into insertion path planning and ablation position planning, which are further simplified into 2D by projections along two orthogonal directions. Here, a heuristic algorithm based on regular arrangement and step-wise adjustment is proposed to implement the 2D planning tasks. Experiments are conducted on patients with liver tumors of different sizes and shapes from multicenter to evaluate the proposed method.
Results
The proposed method automatically generated clinically acceptable RFA plans within 3 min for all cases in the test set and the clinical validation set. All RFA plans of our method achieve 100% treatment zone coverage without damaging the vital organs. Compared with the optimization-based method, the proposed method reduces the planning time by dozens of times while generating RFA plans with similar ablation efficiency.
Conclusion
The proposed method demonstrates a new way to rapidly and automatically generate clinically acceptable RFA plans with multiple clinical constraints. The plans of our method are consistent with the clinical actual plans on almost all cases, which demonstrates the effectiveness of the proposed method and can help reduce the burden on clinicians.




Similar content being viewed by others
References
Garrean S, Hering J, Saied A, Helton WS, Espat NJ (2008) Radiofrequency ablation of primary and metastatic liver tumors: a critical review of the literature. Am J Surg 195:508–520. https://doi.org/10.1016/j.amjsurg.2007.06.024
Benson AB 3rd, Abrams TA, Ben-Josef E et al (2009) NCCN clinical practice guidelines in oncology: hepatobiliary cancers. J Natl Compr Canc Netw: JNCCN 7:350–391. https://doi.org/10.6004/jnccn.2009.0027
Chen MH, Yang W, Yan K et al (2004) Large liver tumors: protocol for radiofrequency ablation and its clinical application in 110 patients—mathematic model, overlapping mode, and electrode placement process. Radiology 232:260–271. https://doi.org/10.1148/radiol.2321030821
Schumann C, Rieder C, Bieberstein J et al (2010) State of the art in computer-assisted planning, intervention, and assessment of liver-tumor ablation. Crit Rev™ Biomed Eng 38: 31–52. https://doi.org/10.1615/CritRevBiomedEng.v38.i1.40
Minami Y, Kudo M (2011) Radiofrequency ablation of hepatocellular carcinoma: a literature review. Int J Hepatol 2011:1–9. https://doi.org/10.4061/2011/104685
Villard C, Soler L, Gangi A (2005) Radiofrequency ablation of hepatic tumors: simulation, planning, and contribution of virtual reality and haptics. Comput Methods Biomech Biomed Eng 8:215–227. https://doi.org/10.1080/10255840500289988
Baegert C, Villard C, Schreck P, Soler L, Gangi A (2007) Trajectory optimization for the planning of percutaneous radiofrequency ablation of hepatic tumors. Comput Aided Surg 12:82–90. https://doi.org/10.3109/10929080701312000
Schumann C, Bieberstein J, Trumm C et al (2010) Fast automatic path proposal computation for hepatic needle placement. In Medical Imaging 2010: Visualization, Image-Guided Procedures, and Modeling. SPIE 7625:478–487. https://doi.org/10.1117/12.844186
Seitel A, Engel M, Sommer CM et al (2011) Computer-assisted trajectory planning for percutaneous needle insertions. Med Phys 38:3246–3259. https://doi.org/10.1118/1.3590374
Jaberzadeh A, Essert C (2016) Pre-operative planning of multiple probes in three dimensions for liver cryosurgery: comparison of different optimization methods. Math Methods Appl Sci 39:4764–4772. https://doi.org/10.1002/mma.3548
Li J, Xu Y, Shen N, Feng L, Ran Z, Deng Z (2020) A practical pretreatment planning method of multiple puncturing for thermal ablation surgery. Biocybern Biomed Eng 40:1469–1485. https://doi.org/10.1016/j.bbe.2020.08.004
Luo M, Jiang H, Shi T (2022) Multi-stage puncture path planning algorithm of ablation needles for percutaneous radiofrequency ablation of liver tumors. Comput Biol Med 145:105506. https://doi.org/10.1016/j.compbiomed.2022.105506
Yang L, Wen R, Qin J, Chui CK, Lim KB, Chang SKY (2010) A robotic system for overlapping radiofrequency ablation in large tumor treatment. IEEE/ASME Trans Mechatron 15:887–897. https://doi.org/10.1109/TMECH.2010.2078827
Giorgi G, Avalle L, Brignone M, Piana M, Caviglia G (2013) An optimisation approach to multiprobe cryosurgery planning. Comput Meth Biomech Biomed Eng 16:885–895. https://doi.org/10.1080/10255842.2011.643469
Torricelli M, Ferraguti F, Secchi C (2013) An algorithm for planning the number and the pose of the iceballs in cryoablation. In: 2013 35th Annual international conference of the IEEE engineering in medicine and biology society (EMBC). IEEE, pp 4949–4952. https://doi.org/10.1109/EMBC.2013.6610658
Ren H, Guo W, Ge SS, Lim W (2014) Coverage planning in computer-assisted ablation based on genetic algorithm. Comput Biol Med 49:36–45. https://doi.org/10.1016/j.compbiomed.2014.03.004
Chen R, Jiang TA, Lu F, Wang K, Kong D (2017) Semiautomatic radiofrequency ablation planning based on constrained clustering process for hepatic tumors. IEEE Trans Biomed Eng 65:645–657. https://doi.org/10.1109/TBME.2017.2712161
He K, Liu X, Shahzad R et al (2021) Advanced deep learning approach to automatically segment malignant tumors and ablation zone in the liver with contrast-enhanced CT. Front Oncol 11:664337. https://doi.org/10.3389/fonc.2021.669437
Meister F, Audigier C, Passerini T et al (2022). Fast automatic liver tumor radiofrequency ablation planning via learned physics model. In: Medical image computing and computer assisted intervention. Springer, Cham, pp 167–176. https://doi.org/10.1007/978-3-031-16449-1_17
Chaitanya K, Audigier C, Balascuta LE, Mansi T (2022) Automatic planning of liver tumor thermal ablation using deep reinforcement learning. In: International conference on medical imaging with deep learning, PMLR 172:219–230
Liang L, Cool D, Kakani N, Wang G, Ding H, Fenster A (2019) Automatic radiofrequency ablation planning for liver tumors with multiple constraints based on set covering. IEEE Trans Med Imaging 39:1459–1471. https://doi.org/10.1109/TMI.2019.2950947
Liang L, Cool D, Kakani N, Wang G, Ding H, Fenster A (2019) Development of a multi-objective optimized planning method for microwave liver tumor ablation. In: International conference on medical image computing and computer-assisted intervention. Springer, Cham, pp 110–118. https://doi.org/10.1007/978-3-030-32254-0_13
Yu P, Fu T, Wu C, Jiang Y, Yang J (2021) Automatic radiofrequency ablation planning for liver tumors: a planning method based on the genetic algorithm with multiple constraints. In: 2021 the 3rd International conference on intelligent medicine and health. Association for Computing Machinery, pp 8–14. https://doi.org/10.1145/3484377.3484379
Li R, Shi Y, Si W et al (2021) Versatile multi-constrained planning for thermal ablation of large liver tumors. Comput Med Imag Graph 94:101993. https://doi.org/10.1016/j.compmedimag.2021.101993
Isensee F, Jaeger PF, Kohl SA, Petersen J, Maier-Hein KH (2021) nnU-Net: a self-configuring method for deep learning-based biomedical image segmentation. Nat Methods 18:203–211. https://doi.org/10.1038/s41592-020-01008-z
Laimer G, Schullian P, Jaschke N et al (2020) Minimal ablative margin (MAM) assessment with image fusion: an independent predictor for local tumor progression in hepatocellular carcinoma after stereotactic radiofrequency ablation. Eur Radiol 30:2463–2472. https://doi.org/10.1007/s00330-019-06609-7
Seror O (2015) Ablative therapies: Advantages and disadvantages of radiofrequency, cryotherapy, microwave and electroporation methods, or how to choose the right method for an individual patient? Diagn Interv Imaging 96:617–624. https://doi.org/10.1016/j.diii.2015.04.007
Funding
This work was supported in part by China NSFC projects (12090024), the National Key Research and Development Program of China (No. 2021ZD0113302 and No. 2019YFC0118101), Zhejiang Provincial Key Research and Development Program (No. 2020C03073), and SJTU Translational Medicine Cross Research Funds (YG2021QN138).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This retrospective study was conducted following ethical approval from the Institutional Review Board of The Third Medical Center of Chinese PLA General Hospital and Daqing Longnan Hospital, and all CT images are anonymized. This paper does not contain any studies with animals performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Supplementary file3 (MP4 10415 KB)
Supplementary file4 (MP4 10422 KB)
Supplementary file5 (MP4 10630 KB)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Li, R., An, C., Wang, S. et al. A heuristic method for rapid and automatic radiofrequency ablation planning of liver tumors. Int J CARS 18, 2213–2221 (2023). https://doi.org/10.1007/s11548-023-02921-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-023-02921-2