Abstract
Purpose
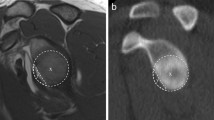
Estimation of glenoid bone loss in CT scans following shoulder dislocation is required to determine the type of surgery needed to restore shoulder stability. This paper presents a novel automatic method for the computation of glenoid bone loss in CT scans.
Methods
The model-based method is a pipeline that consists of four steps: (1) computation of an oblique plane in the CT scan that best matches the glenoid face orientation; (2) selection of the glenoid oblique CT slice; (3) computation of the circle that best fits the posteroinferior glenoid contour; (4) quantification of the glenoid bone loss. The best-fit circle is computed with newly defined Glenoid Clock Circle Constraints.
Results
The pipeline and each of its steps were evaluated on 51 shoulder CT scans (44 patients). Ground truth oblique slice, best-fit circle, and glenoid bone loss measurements were obtained manually from three clinicians. The full pipeline yielded a mean absolute error (%) for the bone loss deficiency of 2.3 ± 2.9 mm (4.67 ± 3.32%). The mean oblique CT slice selection difference was 1.42 ± 1.32 slices, above the observer variability of 1.74 ± 1.82 slices. The glenoid bone loss deficiency measure (%) on the ground truth oblique glenoid CT slice has a mean average error of 0.54 ± 1.03 mm (4.76 ± 3.00%), close to the observer variability of 0.93 ± 1.40 mm (2.98 ± 4.97%).
Conclusion
Our pipeline is the first fully automatic method for the quantitative analysis of glenoid bone loss in CT scans. The computed glenoid bone loss report may assist orthopedists in selecting and planning surgical shoulder dislocation procedures.




Similar content being viewed by others
References
Zacchilli MA, Owens BD (2010) Epidemiology of shoulder dislocations presenting to emergency departments in the United States. J Bone Joint Surg 92(3):542–549
Cutts S, Prempeh M, Drew S (2009) Anterior shoulder dislocation. Ann R Coll Surg Engl 91(1):2–7
Rowe CR, Patel D, Southmayd WW (1978) The Bankart procedure: a long-term end-result study. J Bone Joint Surg 60(1):1–16
Latarjet M (1954) A propos du traitement des luxations recidivantes de l’epaule. Lyon Chir 49:994–997
Chuang TY, Adams CR, Burkhart SS (2008) Use of preoperative three-dimensional computed tomography to quantify glenoid bone loss in shoulder instability. Arthrosc J Arthrosc Relat Surg 24(4):376–382
Dumont GD, Russell RD, Browne MG, Robertson WJ (2012) Area-based determination of bone loss using the glenoid arc angle. Arthrosc J Arthrosc Relat Surg 28(7):1030–1035
Green GL, Arnander M, Pearse E, Tennent D (2022) CT estimation of glenoid bone loss in anterior glenohumeral instability: a systematic review of existing techniques. Bone Joint Open 3(2):114–122
Griffith JF, Antonio GE, Tong CW, Ming CK (2003) Anterior shoulder dislocation: quantification of glenoid bone loss with CT. Am J Roentgenol 180(5):1423–1430
Sugaya H (2010) Instability with bone loss. In: Angelo RL, Esch JC, Ryu RK, eds. AANA advanced arthroscopy: the shoulder, vol 14, pp 136–146
Baudi P, Righi P, Bolognesi D, Rivetta S, Urtoler ER, Guicciardi N, Carrara M (2005) How to identify and calculate glenoid bone deficit. La Chirurgia Degli Organi di Movimento 90(2):145–152
Zhang J, Yan CH, Chui CK, Ong SH (2010) Fast segmentation of bone in CT images using 3D adaptive thresholding. Comput Biol Med 40(2):231–236
Taghizadeh E, Terrier A, Becce F, Farron A, Büchler P (2019) Automated CT bone segmentation using statistical shape modelling and local template matching. Comput Methods Biomech Biomed Eng 22(16):1303–1310
Mahdi FP, Tanaka H, Nobuhara K, Kobashi S (2020) Automatic segmentation of the humerus region in 3-D shoulder CT images using U-Net. Int J Biomed Soft Comput Hum Sci 25(2):67–74
Noguchi S, Nishio M, Yakami M, Nakagomi K, Togashi K (2020) Bone segmentation on whole-body CT using convolutional neural network with novel data augmentation techniques. Comput Biol Med 121:103767
Canny J (1986) A computational approach to edge detection. IEEE Trans Pattern Anal Mach Intell 6:679–698
Yushkevich PA, Gao Y, Gerig G (2016) ITK-SNAP: an interactive tool for semi-automatic segmentation of multi-modality biomedical images. In: proceedings of 38th annual international conference of the IEEE engineering in medicine and biology society, pp, 3342–3345
Linden FV, Schmid K, Rommes E (2007) Philips medical systems. Software product lines in action. Springer, Berlin, pp 233–248
Rabinowitz J, Friedman R, Eichinger JK (2017) Management of glenoid bone loss with anterior shoulder instability: indications and outcomes. Curr Rev Musculoskelet Med 10(4):452–462
Bakshi NK, Cibulas GA, Sekiya JK, Bedi A (2018) A clinical comparison of linear and surface area–based methods of measuring glenoid bone loss. Am J Sports Med 46(10):2472–2477
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent
There was no need for informed consent required for the work reported in this manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Haimi, A., Beyth, S., Gross, M. et al. Automated quantification of glenoid bone loss in CT scans for shoulder dislocation surgery planning. Int J CARS 19, 129–137 (2024). https://doi.org/10.1007/s11548-023-02995-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-023-02995-y