Abstract
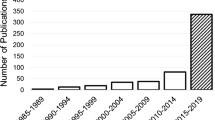
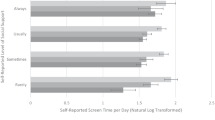
Mental disorders are closely related to deficits in cognitive control. Such cognitive impairments may result in aberrations in mood, thinking, work, body functions, emotions, social engagements and general behaviour. Mental disorders may affect the phenotypic behaviour like eye movements, facial expressions and speech. Furthermore, a close association has been observed within mental disorders and physiological responses emanating from the brain, muscles, heart, eyes, skin, etc. Mental disorders disrupt higher cognitive function, social cognition, control of complex behaviours and regulation of emotion. Cognitive computation may help understand such disruptions for improved decision-making with the help of computers. This study presents a systematic literature review to promulgate state of art computational methods and technologies facilitating automated detection of mental disorders. For this survey, the relevant literature between 2010 and 2021 has been studied. Recommendations of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) model were adopted for identification, screening, validating and inclusion of research literature. The self-diagnosis tools for detection of mental disorders like questionnaires and rating scales are inconsistent and static in nature. They cannot encompass the diversity of mental disorders, inter-individual variability and impact of emotional state of an individual. Furthermore, there are no standard baselines for mental disorders. This situation mandates a multi-faceted approach which may utilise data from physiological signals, behavioural patterns and even data obtained from various online portals like social media to efficiently and effectively detect the prevalence, type and severity of mental disorders.



Similar content being viewed by others
References
Mental disorders: MedlinePlus. https://medlineplus.gov/mentaldisorders.html (accessed 07 Mar 2022).
Ritchie H, Roser M. Mental health. Our World Data. 2018; [Online]. Available: https://ourworldindata.org/mental-health.
James SL, et al. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2018;392(10159):1789–858. https://doi.org/10.1016/S0140-6736(18)32279-7.
Chong SA, Vaingankar JA, Abdin E, Subramaniam M. Mental disorders: employment and work productivity in Singapore. Soc Psychiatry Psychiatr Epidemiol. 2013;48(1):117–23. https://doi.org/10.1007/s00127-012-0526-5.
Too LS, Spittal MJ, Bugeja L, Reifels L, Butterworth P, Pirkis J. The association between mental disorders and suicide: a systematic review and meta-analysis of record linkage studies. J Affect Disord. 2019;259:302–13. https://doi.org/10.1016/j.jad.2019.08.054.
Lund C, et al. Poverty and mental disorders: breaking the cycle in low-income and middle-income countries. Lancet. 2011;378(9801):1502–14. https://doi.org/10.1016/S0140-6736(11)60754-X.
Liu ZH, et al. The prevalence of painful physical symptoms in major depressive disorder: a systematic review and meta-analysis of observational studies. Prog Neuro-Psychopharmacology Biol Psychiatry. 2021;111:110372. https://doi.org/10.1016/J.PNPBP.2021.110372.
Wang Q, Xu R, Volkow ND. Increased risk of COVID-19 infection and mortality in people with mental disorders: analysis from electronic health records in the United States. World Psychiatry. 2021;20(1):124–30. https://doi.org/10.1002/WPS.20806.
Scott KM, et al. Associations between DSM-IV mental disorders and subsequent heart disease onset: beyond depression. Int J Cardiol. 2013;168(6):5293–9. https://doi.org/10.1016/J.IJCARD.2013.08.012.
Razzouk D. Mental health economics: the costs and benefits of psychiatric care. Ment Heal Econ Costs Benefits Psychiatr Care. 2017;1–459. https://doi.org/10.1007/978-3-319-55266-8.
World Health Organisation. SDG indicators — SDG indicators. https://unstats.un.org/sdgs/metadata/?Text=&Goal=3&Target=3.4 (accessed 27 Aug 2021).
Moustgaard H, Bello S, Miller FG, Hróbjartsson A. Subjective and objective outcomes in randomized clinical trials: definitions differed in methods publications and were often absent from trial reports. J Clin Epidemiol. 2014;67(12):1327–34. https://doi.org/10.1016/J.JCLINEPI.2014.06.020.
Lader M. Rating scales in schizophrenia. CNS Drugs 2000. 2012;14(1):23–32. https://doi.org/10.2165/00023210-200014010-00003.
Sajatovic M, Chen P, Young RC. Rating scales in bipolar disorder. Clin Trial Des Challenges Mood Disord. 2015;105–136. https://doi.org/10.1016/B978-0-12-405170-6.00009-9.
Sheehan B. Assessment scales in dementia. Ther Adv Neurol Disord. 2012;5(6):349. https://doi.org/10.1177/1756285612455733.
Fried EI. The 52 symptoms of major depression: lack of content overlap among seven common depression scales. J Affect Disord. 2017;208:191–7. https://doi.org/10.1016/J.JAD.2016.10.019.
Yasuhara A. Correlation between EEG abnormalities and symptoms of autism spectrum disorder (ASD). Brain Dev. 2010;32(10):791–8. https://doi.org/10.1016/J.BRAINDEV.2010.08.010.
Shi T, et al. EEG characteristics and visual cognitive function of children with attention deficit hyperactivity disorder (ADHD). Brain Dev. 2012;34(10):806–11. https://doi.org/10.1016/J.BRAINDEV.2012.02.013.
Pillai V, Kalmbach DA, Ciesla JA. A meta-analysis of electroencephalographic sleep in depression: evidence for genetic biomarkers. Biol Psychiatry. 2011;70(10):912–9. https://doi.org/10.1016/J.BIOPSYCH.2011.07.016.
Narayanan B, et al. Resting state electroencephalogram oscillatory abnormalities in schizophrenia and psychotic bipolar patients and their relatives from the bipolar and schizophrenia network on intermediate phenotypes study. Biol Psychiatry. 2014;76(6):456–65. https://doi.org/10.1016/J.BIOPSYCH.2013.12.008.
Kam JWY, Bolbecker AR, O’Donnell BF, Hetrick WP, Brenner CA. Resting state EEG power and coherence abnormalities in bipolar disorder and schizophrenia. J Psychiatr Res. 2013;47(12):1893–901. https://doi.org/10.1016/J.JPSYCHIRES.2013.09.009.
Olbrich S, Arns M. EEG biomarkers in major depressive disorder: discriminative power and prediction of treatment response. 2013;25(5):604–18. https://doi.org/10.3109/09540261.2013.816269.
Blom EH, Olsson E, Serlachius E, Ericson M, Ingvar M. Heart rate variability (HRV) in adolescent females with anxiety disorders and major depressive disorder. Acta Pædiatrica. 2010;99(4):604–11. https://doi.org/10.1111/J.1651-2227.2009.01657.X.
Liang CS, Lee JF, Chen CC, Chang YC. Reactive heart rate variability in male patients with first-episode major depressive disorder. Prog Neuro-Psychopharmacology Biol Psychiatry. 2015;56:52–7. https://doi.org/10.1016/J.PNPBP.2014.08.004.
Akar SA, Kara S, Latifoğlu F, Bilgiç V. Analysis of heart rate variability during auditory stimulation periods in patients with schizophrenia. J Clin Monit Comput. 2014;29(1):153–62. https://doi.org/10.1007/S10877-014-9580-8.
Kasanuki K, et al. Impaired heart rate variability in patients with dementia with Lewy bodies: efficacy of electrocardiogram as a supporting diagnostic marker. Parkinsonism Relat Disord. 2015;21(7):749–54. https://doi.org/10.1016/J.PARKRELDIS.2015.04.024.
Faurholt-Jepsen M, Kessing LV, Munkholm K. Heart rate variability in bipolar disorder: a systematic review and meta-analysis. Neurosci Biobehav Rev. 2017;73:68–80. https://doi.org/10.1016/J.NEUBIOREV.2016.12.007.
Valenza G, et al. Predicting mood changes in bipolar disorder through heartbeat nonlinear dynamics. IEEE J Biomed Heal Informatics. 2016;20(4):1034–43. https://doi.org/10.1109/JBHI.2016.2554546.
Alam MAU, Roy N, Holmes S, Gangopadhyay A, Galik E. Automated functional and behavioral health assessment of older adults with dementia. Proc. - 2016 IEEE 1st Int. Conf. Connect. Heal. Appl. Syst. Eng. Technol. CHASE. 2016;140–149. https://doi.org/10.1109/CHASE.2016.16.
Greco A, Valenza G, Lanata A, Rota G, Scilingo EP. Electrodermal activity in bipolar patients during affective elicitation. IEEE J Biomed Heal Informatics. 2014;18(6):1865–73. https://doi.org/10.1109/JBHI.2014.2300940.
Sarchiapone M, et al. The association between electrodermal activity (EDA), depression and suicidal behaviour: a systematic review and narrative synthesis. BMC Psychiatry. 2018;18(1):1–27. https://doi.org/10.1186/S12888-017-1551-4.
Pourmohammadi S, Maleki A. Stress detection using ECG and EMG signals: a comprehensive study. Comput Methods Prog Biomed. 2020;193. https://doi.org/10.1016/j.cmpb.2020.105482.
Ghaderi A, Frounchi J, Farnam A. “Machine learning-based signal processing using physiological signals for stress detection”, 2015 22nd Iran. Conf Biomed Eng ICBME. 2016;2015:93–8. https://doi.org/10.1109/ICBME.2015.7404123.
Wijsman J, Grundlehner B, Liu H, Hermens H, Penders J. Towards mental stress detection using wearable physiological sensors. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS. 2011:1798–1801. https://doi.org/10.1109/IEMBS.2011.6090512.
Bubl E, Kern E, Ebert D, Bach M, Tebartz Van Elst L. Seeing gray when feeling blue? Depression can be measured in the eye of the diseased. Biol Psychiatry. 2010;68(2):205–8. https://doi.org/10.1016/J.BIOPSYCH.2010.02.009.
Schwitzer T, Lavoie J, Giersch A, Schwan R, Laprevote V. The emerging field of retinal electrophysiological measurements in psychiatric research: a review of the findings and the perspectives in major depressive disorder. J Psychiatr Res. 2015;70:113–20. https://doi.org/10.1016/J.JPSYCHIRES.2015.09.003.
Berman G, et al. Decreased retinal sensitivity in depressive disorder: a controlled study. Acta Psychiatr Scand. 2018;137(3):231–40. https://doi.org/10.1111/ACPS.12851.
Ma G, et al. Electrocardiographic and electrooculographic responses to external emotions and their transitions in bipolar I and II disorders. Int J Environ Res Public Heal. 2018;15:884. https://doi.org/10.3390/IJERPH15050884.
Hosseinifard B, Moradi MH, Rostami R. Classifying depression patients and normal subjects using machine learning techniques and nonlinear features from EEG signal. Comput Methods Programs Biomed. 2013;109(3):339–45. https://doi.org/10.1016/j.cmpb.2012.10.008.
Li X, Hu B, Sun S, Cai H. EEG-based mild depressive detection using feature selection methods and classifiers. Comput Methods Programs Biomed. 2016;136:151–61. https://doi.org/10.1016/j.cmpb.2016.08.010.
Kim AY, et al. Automatic detection of major depressive disorder using electrodermal activity. Sci Rep. 2018;8(1):1–9. https://doi.org/10.1038/s41598-018-35147-3.
Roh T, Hong S, Yoo HJ. Wearable depression monitoring system with heart-rate variability. 2014 36th Annu Int Conf IEEE Eng Med Biol Soc EMBC. 2014;562–565. https://doi.org/10.1109/EMBC.2014.6943653.
Williamson JR, Quatieri TF, Helfer BS, Ciccarelli G, Mehta DD. “ocal and facial biomarkers of depression based on motor incoordination and timing. AVEC 2014 - Proc 4th Int Work Audio/Visual Emot Challenge, Work MM 2014. 2014. p. 65–72. https://doi.org/10.1145/2661806.2661809.
Mashio Y, Kawaguchi H. Detecting early symptoms of mental health deterioration using handwriting duration parameters. Neuropsychopharmacol Reports. 2020;40(3):246–53. https://doi.org/10.1002/npr2.12123.
Anusha AS, et al. Electrodermal activity based pre-surgery stress detection using a wrist wearable. IEEE J Biomed Heal Informatics. 2020;24(1):92–100. https://doi.org/10.1109/JBHI.2019.2893222.
Pluntke U, Gerke S, Sridhar A, Weiss J, Michel B. Evaluation and classification of physical and psychological stress in firefighters using heart rate variability. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS. 2019;2207–2212. https://doi.org/10.1109/EMBC.2019.8856596.
Bay Ayzeren Y, Erbilek M, Celebi E. Emotional state prediction from online handwriting and signature biometrics. IEEE Access. 2019;7:164759–74. https://doi.org/10.1109/ACCESS.2019.2952313.
Khodayari-Rostamabad A, Reilly JP, Hasey G, Debruin H, MacCrimmon D. Diagnosis of psychiatric disorders using EEG data and employing a statistical decision model. 2010 Annu Int Conf IEEE Eng Med Biol Soc EMBC’10. 2010. p. 4006–4009. https://doi.org/10.1109/IEMBS.2010.5627998.
Liu Y, Du S. Psychological stress level detection based on electrodermal activity. Behav Brain Res. 2018;341:50–3. https://doi.org/10.1016/j.bbr.2017.12.021.
Na KS, Cho SE, Cho SJ. Machine learning-based discrimination of panic disorder from other anxiety disorders. J Affect Disord. 2021;278:1–4. https://doi.org/10.1016/j.jad.2020.09.027.
Cordasco G, Scibelli F, Faundez-Zanuy M, Likforman-Sulem L, Esposito A. “Handwriting and drawing features for detecting negative moods”, in Smart Innovation. Systems and Technologies. 2019;103:73–86.
Erguzel TT, Sayar GH, Tarhan N. Artificial intelligence approach to classify unipolar and bipolar depressive disorders. Neural Comput Appl. 2016;27(6):1607–16. https://doi.org/10.1007/s00521-015-1959-z.
Greco A, Lanata A, Valenza G, Rota G, Vanello N, Scilingo EP. On the deconvolution analysis of electrodermal activity in bipolar patients. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS. 2012;6691–6694. https://doi.org/10.1109/EMBC.2012.6347529.
Du Z, Huang D, Li W, Wang Y. Bipolar disorder recognition via multi-scale discriminative audio temporal representation. AVEC 2018 - Proc. 2018 Audio/Visual Emot. Chall. Work. co-located with MM 2018. 2018. p. 23–30. https://doi.org/10.1145/3266302.3268997.
PRISMA. http://www.prisma-statement.org/Default.aspx (accessed 08 Mar 2022).
Giannakakis G, Grigoriadis D, Giannakaki K, Simantiraki O, Roniotis A, Tsiknakis M. Review on psychological stress detection using biosignals. IEEE Trans Affect Comput. 2019. https://doi.org/10.1109/TAFFC.2019.2927337.
Garcia-Ceja E, Riegler M, Nordgreen T, Jakobsen P, Oedegaard KJ, Tørresen J. Mental health monitoring with multimodal sensing and machine learning: a survey. Pervasive Mob Comput. 2018;51:1–26. https://doi.org/10.1016/j.pmcj.2018.09.003.
de Aguiar Neto FS, Rosa JLG. Depression biomarkers using non-invasive EEG: a review. Neurosci Biobehav Rev. 2019;105:83–93. https://doi.org/10.1016/j.neubiorev.2019.07.021.
Mahato S, Paul S. Electroencephalogram (EEG) signal analysis for diagnosis of major depressive disorder (MDD): a review. Lect Notes Electr Eng. 2019;511:323–35. https://doi.org/10.1007/978-981-13-0776-8_30.
Vasu V, Indiramma M. A survey on bipolar disorder classification methodologies using machine learning. Proc - Int Conf Smart Electron Commun ICOSEC 2020, no. Icosec. 2020. p. 335–340. https://doi.org/10.1109/ICOSEC49089.2020.9215334.
Sabeti M, Katebi S, Boostani R. Entropy and complexity measures for EEG signal classification of schizophrenic and control participants. Artif Intell Med. 2009;47(3):263–74. https://doi.org/10.1016/j.artmed.2009.03.003.
Tekin Erguzel T, Tas C, Cebi M. A wrapper-based approach for feature selection and classification of major depressive disorder-bipolar disorders. Comput Biol Med. 2015;64:127–37. https://doi.org/10.1016/j.compbiomed.2015.06.021.
Mantri S, Patil D,. Agrawal P, Wadhai V. Non invasive EEG signal processing framework for real time depression analysis. IntelliSys 2015 - Proc. 2015 SAI Intell Syst Conf. 2015. p. 518–521. https://doi.org/10.1109/IntelliSys.2015.7361188.
Li X, Hu B, Shen J, Xu T, Retcliffe M. Mild depression detection of college students: an EEG-based solution with free viewing tasks. J Med Syst 2015;39(2). https://doi.org/10.1007/s10916-015-0345-9.
Cai H, Sha X, Han X, Wei S, Hu B. Pervasive EEG diagnosis of depression using Deep Belief Network with three-electrodes EEG collector. In 2016 IEEE International Conference on Bioinformatics and Biomedicine (BIBM). 2016. p. 1239–46. https://doi.org/10.1109/BIBM.2016.7822696.
Cai H, Qu Z, Li Z, Zhang Y, Hu X, Hu B. Feature-level fusion approaches based on multimodal EEG data for depression recognition. Inf Fusion. 2020;59:127–38. https://doi.org/10.1016/j.inffus.2020.01.008.
Mumtaz W, Xia L, Ali SSA, Yasin MAM, Hussain M, Malik AS. Electroencephalogram (EEG)-based computer-aided technique to diagnose major depressive disorder (MDD). Biomed Signal Process Control. 2017;31(2017):108–15. https://doi.org/10.1016/j.bspc.2016.07.006.
Mahato S, Paul S. Detection of major depressive disorder using linear and non-linear features from EEG signals. Microsyst Technol. 2019;25(3):1065–76. https://doi.org/10.1007/s00542-018-4075-z.
Mahato S, Paul S. Classification of depression patients and normal subjects based on electroencephalogram (EEG) signal using alpha power and theta asymmetry. J Med Syst. 2020;44(1):1–8. https://doi.org/10.1007/s10916-019-1486-z.
Bachmann M, Lass J, Hinrikus H. Single channel EEG analysis for detection of depression. Biomed Signal Process Control. 2017;31:391–7. https://doi.org/10.1016/j.bspc.2016.09.010.
Mumtaz W, Qayyum A. A deep learning framework for automatic diagnosis of unipolar depression. Int J Med Inform. 2019;132:103983. https://doi.org/10.1016/j.ijmedinf.2019.103983.
Acharya UR, Oh SL, Hagiwara Y, Tan JH, Adeli H, Subha DP. Automated EEG-based screening of depression using deep convolutional neural network. Comput Methods Programs Biomed. 2018;161:103–13. https://doi.org/10.1016/j.cmpb.2018.04.012.
A. B. et al., “Automated depression detection using deep representation and sequence learning with EEG signals,” J. Med. Syst., vol. 43, no. 7, 2019, [Online]. Available: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L627888073%0Ahttp://dx.doi.org/10.1007/s10916-019-1345-y.
Mumtaz W, Ali SSA, Yasin MAM, Malik AS. A machine learning framework involving EEG-based functional connectivity to diagnose major depressive disorder (MDD). Med Biol Eng Comput. 2018;56(2):233–46. https://doi.org/10.1007/s11517-017-1685-z.
Ghandeharioun A, et al. Objective assessment of depressive symptoms with machine learning and wearable sensors data. 2017 7th Int Conf Affect Comput Intell Interact ACII. 2017;2018:325–32. https://doi.org/10.1109/ACII.2017.8273620.
Sánchez-Reolid R, Martínez-Rodrigo A, López MT, Fernández-Caballero A. Deep support vector machines for the identification of stress condition from electrodermal activity. Int J Neural Syst. 2020;30(7):1–16. https://doi.org/10.1142/S0129065720500318.
Aqajari SAH, Naeini EK, Mehrabadi MA, Labbaf S, Rahmani AM, Dutt N. GSR analysis for stress: development and validation of an open source tool for noisy naturalistic GSR data, no. 1, 2020 [Online]. Available: http://arxiv.org/abs/2005.01834.
Melillo P, Formisano C, Bracale U, Pecchia L. Classification tree for real-life stress detection using linear heart rate variability analysis. Case study: students under stress due to university examination. IFMBE Proc. 2013;39:477–80. https://doi.org/10.1007/978-3-642-29305-4_126.
Wang JS, Lin CW, Yang YTC. A k-nearest-neighbor classifier with heart rate variability feature-based transformation algorithm for driving stress recognition. Neurocomputing. 2013;116:136–43. https://doi.org/10.1016/j.neucom.2011.10.047.
Karthikeyan P, Murugappan M, Yaacob S. Analysis of stroop colorword test-based human stress detection using electrocardiography and heart rate variability signals. Arab J Sci Eng. 2012;39(3):1835–47. https://doi.org/10.1007/s13369-013-0786-8.
Castaldo R, Xu W, Melillo P, Pecchia L, Santamaria L, James C. Detection of mental stress due to oral academic examination via ultra-short-term HRV analysis. Proc Annu Int Conf IEEE Eng Med Biol Soc EMBS. 2016;3805–8. https://doi.org/10.1109/EMBC.2016.7591557.
Rizwan MF, Farhad R, Mashuk F, Islam F, Imam MH. Design of a biosignal based stress detection system using machine learning techniques. 1st Int Conf Robot Electr Signal Process Tech (ICREST). 2019;364–8. https://doi.org/10.1109/ICREST.2019.8644259.
Byun S, et al. Detection of major depressive disorder from linear and nonlinear heart rate variability features during mental task protocol. Comput Biol Med. 2019;112:103381. https://doi.org/10.1016/j.compbiomed.2019.103381.
Kuang D, et al. Depression recognition according to heart rate variability using Bayesian Networks. J Psychiatr Res. 2017;95:282–7. https://doi.org/10.1016/j.jpsychires.2017.09.012.
Coutts LV, Plans D, Brown AW, Collomosse J. Deep learning with wearable based heart rate variability for prediction of mental and general health. J Biomed Inform. 2020;112:103610. https://doi.org/10.1016/j.jbi.2020.103610.
Mariya LP, Kumareshan N. Depression detection using comparative analysis of QRS detection algorithms and HRV of ECG signal implemented on MATLAB and Verilog. J Phys Conf Ser. 1916;1:2021. https://doi.org/10.1088/1742-6596/1916/1/012018.
Kim EY, Lee MY, Kim SH, Ha K, Kim KP, Ahn YM. Diagnosis of major depressive disorder by combining multimodal information from heart rate dynamics and serum proteomics using machine-learning algorithm. Prog Neuro-Psychopharmacology Biol Psychiatry. 2017;76:65–71. https://doi.org/10.1016/j.pnpbp.2017.02.014.
Benson PJ, Beedie SA, Shephard E, Giegling I, Rujescu D, St D. Clair, “Simple viewing tests can detect eye movement abnormalities that distinguish schizophrenia cases from controls with exceptional accuracy.” Biol Psychiatry. 2012;72(9):716–24. https://doi.org/10.1016/J.BIOPSYCH.2012.04.019.
Meng H, Huang D, Wang H, Yang H, Al-Shuraifi M, Wang Y. Depression recognition based on dynamic facial and vocal expression features using partial least square regression. AVEC 2013 - Proc 3rd ACM Int Work Audio/Visual Emot Chall. 2013. p. 21–9. https://doi.org/10.1145/2512530.2512532.
Zhu Y, Shang Y, Shao Z, Guo G. Automated depression diagnosis based on deep networks to encode facial appearance and dynamics. IEEE Trans Affect Comput. 2018;9(4):578–84. https://doi.org/10.1109/TAFFC.2017.2650899.
Alghowinem S, et al. Multimodal depression detection: fusion analysis of paralinguistic, head pose and eye gaze behaviors. IEEE Trans Affect Comput. 2018;9(4):478–90. https://doi.org/10.1109/TAFFC.2016.2634527.
Srimadhur NS, Lalitha S. An end-to-end model for detection and assessment of depression levels using speech. Procedia Comput Sci. 2020;171:12–21. https://doi.org/10.1016/J.PROCS.2020.04.003.
Bishay M, Palasek P, Priebe S, Patras I. SchiNet: automatic estimation of symptoms of schizophrenia from facial behaviour analysis. IEEE Trans Affect Comput. 2019;12(4):949–61. https://doi.org/10.1109/taffc.2019.2907628.
Singh J, Goya G. Decoding depressive disorder using computer vision. Multimed Tools App. 2020;80(6):8189–212. https://doi.org/10.1007/S11042-020-10128-9.
Lee SC, Chen KW, Liu CC, Kuo CJ, Hsueh IP, Hsieh CL. Using machine learning to improve the discriminative power of the FERD screener in classifying patients with schizophrenia and healthy adults. J Affect Disord. 2021;292:102–7. https://doi.org/10.1016/j.jad.2021.05.032.
Rosenblum S, Werner P, Dekel T, Gurevitz I, Heinik J. Handwriting process variables among elderly people with mild Major Depressive Disorder: a preliminary study. Aging Clin Exp Res. 2010;22(2):141–7. https://doi.org/10.1007/BF03324787.
Likforman-Sulem L, Esposito A, Faundez-Zanuy M, Clemencon S, Cordasco G. EMOTHAW: a novel database for emotional state recognition from handwriting and drawing. IEEE Trans Human-Machine Syst. 2017;47(2):273–84. https://doi.org/10.1109/THMS.2016.2635441.
Nolazco-Flores JA, Faundez-Zanuy M, Velázquez-Flores OA, Del-Valle-soto C, Cordasco G, Esposito A. Mood state detection in handwritten tasks using PCA–mFCBF and automated machine learning. Sensors. 2022;22(4):1–22. https://doi.org/10.3390/s22041686.
Hindra K, Maslov AV, Pechenizkiy M. Stress detection from speech and Galvanic Skin Response signals. Proc 26th IEEE Int Symp Comput Med Syst. 2013. p. 579. https://doi.org/10.1109/cbms.2013.6627790.
Sun F, Kuo C, Cheng H, Buthpitiya S. Activity-aware mental stress detection. In International Conference on Mobile Computing, Applications, and Services. 2012. p. 282–301.
Smets E, et al. Comparison of machine learning techniques for psychophysiological stress detection. Pervasive Comput Paradig Ment Heal. 2019;604:147–56. https://doi.org/10.1007/978-3-319-32270-4.
Sandulescu V, Andrews S, Ellis D, Bellotto N, Mozos OM. Stress detection using wearable physiological sensors. Artif Comput Biol Med IWINAC 2015;9107:526–532. 2015;9107:526–32. https://doi.org/10.1007/978-3-319-18914-7.
Bobade P, Vani M. Stress detection with machine learning and deep learning using multimodal physiological data. Proc 2nd Int Conf Inven Res Comput Appl ICIRCA. 2020. p. 51–7. https://doi.org/10.1109/ICIRCA48905.2020.9183244.
Ding X, Yue X, Zheng R, Bi C, Li D, Yao G. Classifying major depression patients and healthy controls using EEG, eye tracking and galvanic skin response data. J Affect Disord. 2019;251:156–61. https://doi.org/10.1016/j.jad.2019.03.058.
Tazawa Y, et al. Evaluating depression with multimodal wristband-type wearable device: screening and assessing patient severity utilizing machine-learning. Heliyon. 2020;6(2):e03274. https://doi.org/10.1016/j.heliyon.2020.e03274.
Okubo M, Kobayashi A, Ishikawa K. A fake smile thwarts cheater detection. J Nonverbal Behav. 2012;36(3):217–25. https://doi.org/10.1007/S10919-012-0134-9.
Littlewort GC, Bartlett MS, Lee K. Automatic coding of facial expressions displayed during posed and genuine pain. Image Vis Comput. 2009;27(12):1797–803. https://doi.org/10.1016/J.IMAVIS.2008.12.010.
Gosselin P, Perron M, Beaupré M. The voluntary control of facial action units in adults. Emotion. 2010;10(2):266–71. https://doi.org/10.1037/A0017748.
Jalil NA, Yunus RM, Said NS. Environmental colour impact upon human behaviour: a review. Procedia - Soc Behav Sci. 2012;35:54–62. https://doi.org/10.1016/J.SBSPRO.2012.02.062.
Kanai R, Rees G. The structural basis of inter-individual differences in human behaviour and cognition. Nat Rev Neurosci. 2011;12(4):231–42. https://doi.org/10.1038/nrn3000.
Basu S, Bag A, Aftabuddin M, Mahadevappa M, Mukherjee J, Guha R. Effects of emotion on physiological signals. 2016 IEEE Annu. India Conf. INDICON 2016. 2017. https://doi.org/10.1109/INDICON.2016.7839091.
Kondacs A, Szabó M. Long-term intra-individual variability of the background EEG in normals. Clin Neurophysiol. 1999;110(10):1708–16. https://doi.org/10.1016/S1388-2457(99)00122-4.
Hu X, Chen J, Wang F, Zhang D. Ten challenges for EEG-based affective computing. 2019;5(1):1–20. https://doi.org/10.1177/2096595819896200.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Conflict of Interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Singh, J., Hamid, M.A. Cognitive Computing in Mental Healthcare: a Review of Methods and Technologies for Detection of Mental Disorders. Cogn Comput 14, 2169–2186 (2022). https://doi.org/10.1007/s12559-022-10042-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12559-022-10042-2