Abstract
Purpose
The early detection of organ failure mitigates the risk of post-intensive care syndrome and long-term functional impairment. The aim of this study is to predict organ failure in real-time for critical care patients based on a data-driven and knowledge-driven machine learning method (DKM) and provide explanations for the prediction by incorporating a medical knowledge graph.
Methods
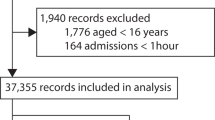
The cohort of this study was a subset of the 4,386 adult Intensive Care Unit (ICU) patients from the MIMIC-III dataset collected between 2001 and 2012, and the primary outcome was the Delta Sequential Organ Failure Assessment (SOFA) score. A real-time Delta SOFA score prediction model was developed with two key components: an improved deep learning temporal convolutional network (S-TCN) and a graph-embedding feature extraction method based on a medical knowledge graph. Entities and relations related to organ failure were extracted from the Unified Medical Language System to build the medical knowledge graph, and patient data were mapped onto the graph to extract the embeddings. We measured the performance of our DKM approach with cross-validation to avoid the formation of biased assessments.
Results
An area under the receiver operating characteristic curve (AUC) of 0.973, a precision of 0.923, a NPV of 0.989, and an F1 score of 0.927 were achieved using the DKM approach, which significantly outperformed the baseline methods. Additionally, the performance remained stable following external validation on the eICU dataset, which consists of 2,816 admissions (AUC = 0.981, precision = 0.860, NPV = 0.984). Visualization of feature importance for the Delta SOFA score and their relationships on the basic clinical medical (BCM) knowledge graph provided a model explanation.
Conclusion
The use of an improved TCN model and a medical knowledge graph led to substantial improvement in prediction accuracy, providing generalizability and an independent explanation for organ failure prediction in critical care patients. These findings show the potential of incorporating prior domain knowledge into machine learning models to inform care and service planning.




Similar content being viewed by others
References
Carrico CJ, Meakins JL, Marshall J, et al. Multiple-organ-failure syndrome. Arch Surg. 1986;121(2):196–208.
Lambden S, Laterre PF, Levy MM, et al. The SOFA score—development, utility and challenges of accurate assessment in clinical trials. Crit Care. 2019;23(1):1–9.
Kim HI, Park S. Sepsis: early recognition and optimized treatment. Crit Care Med. 2019;82(1):6–14.
Lauritsen SM, Kristensen M, Olsen MV, Larsen MS, Lauritsen KM, Jørgensen MJ, Lange J, Thiesson B. Explainable artificial intelligence model to predict acute critical illness from electronic health records. Nat Commun. 2020;11(1):1–11.
Yang M, Liu C, Wang X, et al. An explainable artificial intelligence predictor for early detection of sepsis. Crit Care Med. 2020;48(11):e1091–6.
Chen W, Wang S, Long G, et al. Dynamic illness severity prediction via multi-task rnns for intensive care unit. In: IEEE International Conference on Data Mining (ICDM)IEEE, pp. 917–922; 2018
Zhang X, Zhao Y, Callcut R, et al. Multiple Organ Failure Prediction with Classifier-Guided Generative Adversarial Imputation Networks. 2021, p^pp arXiv:2106.11878
Antoniadi AM, Du Y, Guendouz Y, et al. Current challenges and future opportunities for XAI in machine learning-based clinical decision support systems: a systematic review. Appl Sci. 2021;11(11):5088.
Feldmann C, Philipps M, Bajorath J. Explainable machine learning predictions of dual-target compounds reveal characteristic structural features. Sci Rep. 2021;11(1):1–11.
Durán JM. Dissecting scientific explanation in AI (sXAI): a case for medicine and healthcare. Artif Intell. 2021;297:103498.
Rotmensch M, Halpern Y, Tlimat A, et al. Learning a health knowledge graph from electronic medical records. Sci Rep. 2017;7(1):1–11.
Li L, Wang P, Yan J, et al. Real-world data medical knowledge graph: construction and applications. Artif Intell Med. 2020;103:101817.
Collins GS, Reitsma JB, Altman DG, et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): the TRIPOD statement. J Br Surg. 2015;102(3):148–58.
Vincent J-L, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intens Care Med. 1996;22:707–10.
Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Benesty J, Chen J, Huang Y, et al. Pearson correlation coefficient. In: Noise reduction in speech processing
Lipton ZC, Kale D, Wetzel R. Directly modeling missing data in sequences with rnns: Improved classification of clinical time series. In: Machine learning for healthcare conferencePMLR, pp. 253–270; 2016
McCray AT, Razi AM, Bangalore AK, et al., The UMLS Knowledge Source Server: a versatile Internet-based research tool. In: Proceedings of the AMIA Annual Fall SymposiumAmerican Medical Informatics Association, pp. 164–168; 1996
Donnelly K. SNOMED-CT: the advanced terminology and coding system for eHealth. Stud Health Technol Inform. 2006;121:279.
Brown EG, Wood L. Wood SJDs: the medical dictionary for regulatory activities (MedDRA). Drug Saf. 1999;20(2):109–17.
Liu S, Ma W, Moore R, et al. RxNorm: prescription for electronic drug information exchange. IT Prof. 2005;7(5):17–23.
Fragoso G, de Coronado S, Haber M, et al. Overview and utilization of the NCI thesaurus. Compar Funct Genomics. 2004;5(8):648–54.
Abbreviations Used in Data Elements-2021AB Release. Available at: https://www.nlm.nih.gov/research/umls/knowledge_sources/metathesaurus/release/abbreviations.html. Accessed 12 Oct 2021
Bordes A, Usunier N, Garcia-Duran A, et al: Translating embeddings for modeling multi-relational data. In: Advances in neural information processing systems; 2013
Lea C, Vidal R, Reiter A, et al., Temporal convolutional networks: a unified approach to action segmentation. In: European Conference on Computer Vision (ECCV). Springer, Cham, pp. 47–54; 2016
He K, Zhang X, Ren S, et al., Deep residual learning for image recognition. In: Proceedings of the IEEE Conference on Computer Vision and Pattern Recognition (CVPR), pp 770–778; 2016
Tarjan R. Depth-first search and linear graph algorithms. SIAM J Comput. 1972;1(2):146–60.
Wijnberge M, Geerts BF, Hol L, et al. Effect of a machine learning–derived early warning system for intraoperative hypotension vs standard care on depth and duration of intraoperative hypotension during elective noncardiac surgery: the HYPE randomized clinical trial. JAMA. 2020;323(11):1052–60.
Deng S, Zhang N, Zhang W, et al., Knowledge-driven stock trend prediction and explanation via temporal convolutional network. In: Proceedings of the World Wide Web Conference (WWW), pp. 678–685; 2019
Wang M, Zhang J, Liu J, et al., Pdd graph: Bridging electronic medical records and biomedical knowledge graphs via entity linking. In: International Semantic Web Conference (ISWC). Springer, pp. 219–227; 2017
Gong F, Wang M, Wang H, et al., SMR: Medical Knowledge Graph Embedding for Safe Medicine Recommendation. 2017, p^pp arXiv:1710.05980
Sharma S, Santra B, Jana A, et al., Incorporating Domain Knowledge into Medical NLI using Knowledge Graphs. 2019, p^pp arXiv:1909.00160
Ma F, Gao J, Suo Q, et al., Risk prediction on electronic health records with prior medical knowledge. In: Proceedings of the ACM SIGKDD International Conference on Knowledge Discovery & Data Mining (KDD), pp. 1910–1919; 2018
Bai T, Vucetic S. Improving medical code prediction from clinical text via incorporating online knowledge sources. In: Proceedings of the World Wide Web Conference (WWW), pp 72–82; 2019
Rajkomar A, Dean J, Kohane I. Machine learning in medicine. N Engl J Med. 2019;380(14):1347–58.
Shickel B, Tighe PJ, Bihorac A, et al. Deep EHR: a survey of recent advances in deep learning techniques for electronic health record (EHR) analysis. IEEE J Biomed Health Inform. 2017;22(5):1589–604.
Chen P, Dong W, Wang J, et al. Interpretable clinical prediction via attention-based neural network. BMC Med Inform Decis Mak. 2020;20(3):1–9.
Rajabi E, Etminani K. Towards a knowledge graph-based explainable decision support hystem in Healthcare. Stud Health Technol Inform. 2021;281:502–3.
Wang Q, Mao Z, Wang B, et al. Knowledge graph embedding: a survey of approaches and applications. IEEE Trans Knowl Data Eng. 2017;29(12):2724–43.
Fleuren LM, Klausch TL, Zwager CL, et al. Machine learning for the prediction of sepsis: a systematic review and meta-analysis of diagnostic test accuracy. Intens Care Med. 2020;46(3):383–400.
Funding
The study was supported by the National Key Research and Development Program of China (No. 2022YFF0712400), the National Natural Science Foundation of China (81901842, 61906037, 62276063), Natural Science Foundation of Hunan Province (2021JJ40936), and China Primary Health Care Foundation (YLGX-WS-2020003).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ma, X., Wang, M., Lin, S. et al. Knowledge and data-driven prediction of organ failure in critical care patients. Health Inf Sci Syst 11, 7 (2023). https://doi.org/10.1007/s13755-023-00210-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s13755-023-00210-5