Abstract
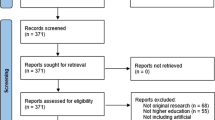
The aim of this study was to identify problems arisen by conventional curricula, the guidelines for development of an appropriate educational model for 21st century, and the advantages and disadvantages of the last two curricular models. The medical education literature published from 1995 through 2002 of four reputable journals in medical education were searched (Academic Medicine, Teaching and Learning in Medicine, Medical Education, and Medical Teacher). First the possibly best articles were identified. During the second screening process 76 of 180 articles were found to be highly relevant to our questions. A review of the chosen articles revealed a concept map which starts from currently applied hypothetical-deductive reasoning (HDR)-based curricula in many medical schools all around the world. Results revelaed that continuing cyclical process might be time consuming, enhance burden of faculty and might be stressful for students involved. Current issues in health care system are possibly attributable to current HDR-based curricular models including PBL. Advantages of reiterative PBL theory can not be denied, but it appears that its limited application should be mainly seen in some academic classes to develop some generic transferable skills simultaneously with other teaching methods. Therefore vast application of HDR in clinical settings is not recommended according to our study. However the relationships demonstrated between factors and outcomes mentioned in the concept map can be used to run some new studies to test some hypotheses.

Similar content being viewed by others
References
Kizer, K. W., The national quality forum seeks to improve heath care. Acad. Med. 75(4):320–322, 2000.
General Medical Council, Tomorrow's Doctors: Recommendation on Undergraduate Medical Education. GMC: UK, 1993.
Abrahamson, S., Time to return medical schools to their primary purpose: Education. Acad. Med. 71(4):343–347, 1996.
Barrows, H. S., and Pickell, G. C., Developing Clinical Problem-Solving Skills: A Guide to More Effective Diagnosis and Treatment. Norton Medical Books: London, 1991.
Coderre, S., Mandin, H., Harasym, P. H., and Fick, G. H., Diagnostic reasoning strategies and diagnostic success. Med. Educ. 37(8):695–703, 2003.
Papa, F. J., and Harasym, P. H., Medical curriculum reform in North America, 1765 to the present: A cognitive science perspective. Acad. Med. 74(2):154–164, 1999.
Gigerenzer, G., Bounded rationality: Models of fast and frugal inference. Swiss. J. Econ. Stat. 133:201–218, 1997.
Colliver, J. A., Effectiveness of problem-based learning curricula: Research and theory. Acad. Med. 75(3):259–266, 2000.
Distlehorst, L. H., and Robbs, R. S., A comparison of problem-based learning and standard curriculum students: Three years of retrospective data. Teach. Learn. Med. 10(3):131–137, 1998.
Woloschuk, W., Harasym, P., Mandin, H., and Jones, A., Use of scheme-based problem solving: an evaluation of the implementation and utilization of schemes in a clinical presentation curriculum. Med. Educ. 34(6):437–442, 2000.
Azer, S. A., Problem-based learning. Challenges, barriers and outcome issues. Saudi Med. J. 22(5):389–397, 2001.
Lester, H., Tritter, J. Q., Medical error: A discussion of the medical construction of error and suggestions for reforms of medical education to decrease error. Med. Educ. 35(9):855–861, 2001.
Berkson, L., Problem-based learning: have the expectations been met? Acad. Med. 68(10 Suppl.):S79–S88, 1993.
Mangione, S., The teaching of chest auscultation in U.S. internal medicine and family practice medicine residencies. Acad. Med. 74(10 Suppl):90–92, 1999.
Mangione, S., The teaching of cardiac auscultation during internal medicine and family medicine training A nationwide comparison. Acad. Med. 73(10 Suppl):10–12, 1998.
Raghoebar-Krieger, H. M. J., Sleijfer, Dth, Hofstee, W. K. B., et al., The availability of diseases for medical students in a university hospital medical teacher. 23(3):258–262, 2001.
Cohen, J. J., Medical schools and teaching hospitals serving the needs of America's communities. Acad. Med. 73(11):1177, 1998.
Lingard, L. A., and Haber, R. J., What Do we Mean by “Relevance”? A clinical and rhetorical definition with implications for teaching and learning the case-presentation format. Acad. Med. 74(10 Suppl):124–127, 1999.
Friedman, M. H., Connell, K. J., Bordage, G., et al., Medical student errors in making a diagnosis. Acad. Med. 73(10 Suppl):19–21, 1998.
Patel, V. L., Groen, G. J., and Norman, G. R., Effects of conventional and problem-based medical curricula on problem solving. Acad. Med. 66(7):380–389, 1991.
Rudy, D. W., Ramsbottom-Lucier, M., Griffith, C. H., III, et al., A pilot study Assessing the Influences of charge data and group process on diagnostic test ordering by residents. Acad. Med. 76(6):635–637, 2001.
Southgate, L., Cox, J., David, T., et al., The assessment of poorly performing doctors: The development of the assessment programs for the general medical council's performance procedures. Med. Educ. 35(12 Suppl 1):2–8, 2001.
Board, P., and Mercer, M., A survey of the Basic practical skills of final year medical students in one UK Medical school. Med. Teach. 20(2):104–148, 1998.
Rosal, M. C., Ockene, I. S., Ockene, J. K., et al., A longitudinal study of students’ depression at one medical school. Acad. Med. 72(6):542–546, 1997.
Cusimano, M. D., Yonke, A. M., and Tucker, W. S., An analysis of attrition from Canadian neurosurgery residency programs. Acad. Med. 74(8):925–931, 1999.
Sales, A. D., Pade, C., and Vinson, D. C., What do family patients think about medical students participation in their Health care? Acad. Med. 74(5):550–552, 1999.
Mandin, H., Jones, A., Woloschuk, W., etc. Helping students learn to think like experts when solving clinical problems. Acad. Med. 72(3):173–179, 1997.
Mandin, H., Harasym, P., Eagle, C., and Watanabe, M., Developing a “clinical presentation” curriculum at the University of Calgary. Acad. Med. 70(3):186–193, 1995.
Acknowledgement
We would like to thank the following authorities and colleagues in the following Institutes and organizations: Prof. Peter H. Harasym, PhD, Dept. of Community Health Sciences, University Of Calgary, Canada for technical support; Dr. Mohammed A. Mohagheghi, the Deputy Minister for Educational and Student Affairs, Ministry of Health and Medical Education, Iran; Dr. Mubasher Sheikh WHO representative in Iran; Members of Center for Adaptive Behavior and Cognition, Max Planck Institute, Berlin, Germany for their guidance on the recent cognitive theories of reasoning and decision-making especially the “Theory of Bounded Rationality”: Peter M Todd,PhD; Prof. Gerd Gigerenzer, PhD; Ulrich Hoffrage, PhD. The author Hakan Yaman and this article has been supported by the Akdeniz University Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Additional information
A preliminary form of this article has been presented at the the first Asia-Pacific Medical Education Congress, Singapore 2003 (Which kind of curriculum is more effective: Inductive or deductive one?: 123.).
Rights and permissions
About this article
Cite this article
Haeri, A., Hemmati, P. & Yaman, H. What Kind of Curriculum Can Better Address Community Needs? Problems Arisen by Hypothetical-Deductive Reasoning. J Med Syst 31, 173–177 (2007). https://doi.org/10.1007/s10916-007-9052-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-007-9052-5