Abstract
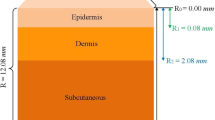
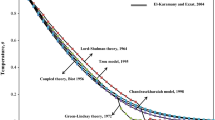
Understanding the mechanisms of skin behavior under thermal shock is crucial for medical treatments. However, no reasonable criteria are available for the maximum thermal loadings that skin tissue can survive. To address this, in this paper we analyzed thermal and neural behaviors of skin tissue exposed to thermal loadings by introducing the thermal shock resistance (a parameter widely used for engineering materials) of skin for the first time. Skin thermal shock resistance was analyzed according to two distinct criteria: (1) maximum local temperature at epidermis-dermis (ED) interface defined as the thermal threshold of skin thermal pain; (2) maximum thermal damage at ED interface defined as the first degree burn where irreversible skin damage occurs. Numerical simulation was performed and the results show that the thermal shock resistance of skin tissue depends on the Biot number (which characterizes the features of thermal shock). These results indicate that skin thermal shock resistance can be used as an efficient tool to predict thermal damage (e.g., burn) and the corresponding pain level induced by noxious thermal loadings (e.g., clinical thermal treatments).




Similar content being viewed by others
References
D’Souza, A. L., Nelson, N. G., and McKenzie, L. B., Pediatric burn injuries treated in US Emergency Departments between 1990 and 2006. Pediatrics 124:1424–1430, 2009. doi:10.1542/peds.2008-2802.
Stewart, D. A., Gowrishankar, T. R., and Weaver, J. C., Skin heating and injury by prolonged millimeter-wave exposure: theory based on a skin model coupled to a whole body model and local biochemical release from cells at supraphysiologic temperatures. IEEE Trans. Plasma. Sci. 34:1480–1493, 2006.
Stec, B., Dobrowolski, A., and Susek, W. Institute of Electrical and Electronics Engineers Inc., New York, NY 10016-5997, United States, 603–606.
Weiss, R. A., Weiss, M. A., Munavalli, G., and Beasley, K. L., Monopolar radiofrequency facial tightening: a retrospective analysis of efficacy and safety in over 600 treatments. J. Drugs Dermatol. 5:707–712, 2006.
Sadick, N. S., and Shaoul, J., Hair removal using a combination of conducted radiofrequency and optical energies–an 18-month follow-up. J. Cosmet. Laser Ther. 6:21–26, 2004.
Goldberg, D. J., Laser- and light-based hair removal: an update. Expert Rev. Med. Devices 4:253–260, 2007.
Bernstein, E. F., The new-generation, high-energy, 595 nm, long pulse-duration, pulsed-dye laser effectively removes spider veins of the lower extremity. Lasers Surg. Med. 39:218–224, 2007.
Tay, Y. K., Kwok, C., and Tan, E., Non-ablative 1, 450-nm diode laser treatment of striae distensae. Lasers Surg. Med. 38:196–199, 2006.
Pearse, H. E., Problems in the experimental study of flash burns. Science 110:444–444, 1949.
Pearse, H. E., Payne, J. T., and Hogg, L., The experimental study of flash-burns. Ann. Surg. 130:774–789, 1949.
Torvi, D. A., and Dale, J. D., A finite-element model of skin subjected to a flash fire. J. Biomech. Eng.-T. Asme 116:250–255, 1994.
Maichrzak, E., Mochnacki, B., and Jasinski, M. Numerical modelling of bioheat transfer in multi-layer skin tissue domain subjected to a flash fire. Computational Fluid and Solid Mechanics 2003, Vols 1 and 2, Proceedings, 1766–1770 2443 (2003).
Wu, Y. C., Material properties criteria for thermal safety. J. Mater. 7:573–579, 1972.
Subramanian, B., and JC, C., Safe touch temperatures for hot plates. J. Biomech. Eng.-T. Asme 120:727–736, 1998.
Lu, T. J., and Fleck, N. A., The thermal shock resistance of solids. Acta Mater. 46:4755–4768, 1998.
Xu, F., Wen, T., Seffen, K. A., and Lu, T. J., Biothermomechanics of skin tissue. J. Mech. Phys. Solids 56:1852–1884, 2008.
Pennes, H. H., Analysis of tissue and arterial blood temperatures in the resting human forearm. J. Appl. Physiol. 1:93–122, 1948.
Xu, F., Wen, T., Lu, T. J., and Seffen, K. A., Skin biothermomechanics for medical treatments. J. Mech. Behav. Biomed. Mater. 1:172–187, 2008. doi:S1751-6161(07)00030-6. [pii] 10.1016/j.jmbbm.2007.09.001.
Xu, F., Seffen, K. A., and Lu, T. J., Non-Fourier analysis of skin biothermomechanics. Int. J. Heat Mass Tran. 51:2237–2259, 2008.
Henriques, F., Jr., and Moritz, A., Studies of thermal injury: I. The conduction of heat to and through skin and the temperatures attained therein. A theoretical and an experimental investigation*. Am. J. Pathol. 23:530, 1947.
Schulz, J. T., III, Tompkins, R. G., and Burke, J. F., Artificial skin. Annu. Rev. Med. 51:231–244, 2000.
Henriques, F. C., Study of thermal injuries V. The predictability and the significance of thermally induced rate processes leading to irreversible epidermal injury. Arch. Pathol. 43:489–502, 1947.
Xu, F., Wen, T., Lu, T. J., and Seffen, K. A. Modeling of nociceptor transduction in skin thermal pain sensation. J. Biomech. Eng. 130, 2008.
Patapoutian, A., Peier, A. M., Story, G. M., and Viswanath, V., Thermo TRP channels and beyond: mechanisms of temperature sensation. Nat. Rev. Neurosci. 4:529–539, 2003.
Xu, F., Wen, T., Lu, T. J., and Seffen, K. A., Modeling of skin thermal pain: a preliminary study. J. Appl. Math. Comput. 205:37–46, 2008.
Xu, F., Wen, T., Lu, T. J., and Seffen, K. A., Modelling of nociceptor transduction in skin thermal pain sensation. J. Biomech. Eng. 130:1–13, 2008.
Xu, F., Lu, T. J., and Seffen, K. A., Skin thermal pain modeling. a holistic method. J. Therm. Biol. 33:223–237, 2008.
Arendt-Nielsen, L., and Chen, A. C. N., Lasers and other thermal stimulators for activation of skin nociceptors in humans. Neurophysiologie Clinique/Clinical Neurophysiology 33:259–268, 2003.
Acknowledgements
This work is supported by the National Natural Science Foundation of China (10825210), the National 111 Project of China (B06024), and the National Basic Research Program of China (2006CB601202).
Author information
Authors and Affiliations
Corresponding authors
Additional information
ZhiBin Fan and Xiao Zhai contributed equally to this work.
Rights and permissions
About this article
Cite this article
Fan, Z., Zhai, X., Zhou, L. et al. Thermal Shock Resistance of Skin Tissue. J Med Syst 35, 863–867 (2011). https://doi.org/10.1007/s10916-010-9503-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10916-010-9503-2