Abstract
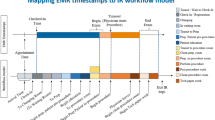
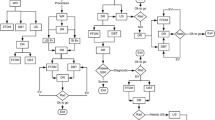
The process of lung cancer care from initial lesion detection to treatment is complex, involving multiple steps, each introducing the potential for substantial delays. Identifying the steps with the greatest delays enables a focused effort to improve the timeliness of care-delivery, without sacrificing quality. We retrospectively reviewed clinical events from initial detection, through histologic diagnosis, radiologic and invasive staging, and medical clearance, to surgery for all patients who had an attempted resection of a suspected lung cancer in a community healthcare system. We used a computer process modeling approach to evaluate delays in care delivery, in order to identify potential ‘bottlenecks’ in waiting time, the reduction of which could produce greater care efficiency. We also conducted ‘what-if’ analyses to predict the relative impact of simulated changes in the care delivery process to determine the most efficient pathways to surgery. The waiting time between radiologic lesion detection and diagnostic biopsy, and the waiting time from radiologic staging to surgery were the two most critical bottlenecks impeding efficient care delivery (more than 3 times larger compared to reducing other waiting times). Additionally, instituting surgical consultation prior to cardiac consultation for medical clearance and decreasing the waiting time between CT scans and diagnostic biopsies, were potentially the most impactful measures to reduce care delays before surgery. Rigorous computer simulation modeling, using clinical data, can provide useful information to identify areas for improving the efficiency of care delivery by process engineering, for patients who receive surgery for lung cancer.





Similar content being viewed by others
References
American Cancer Society, Cancer facts & figures 2016. Atlanta: American Cancer Society, 2016.
http://www.cancer.org/cancer/lungcancer-non-smallcell/detailedguide/non-small-cell-lung-cancerkey-statistics, 2015. Retrieved on June 6, 2015.
Little, A.G., Rusch, V.W., Bonner, J.A., et al., Patterns of surgical care of lung cancer patients. Ann Thorac Surg. 80:2051–2056; discussion 2056, 2005.
Singh, H., Hirani, K., Kadiyala, H., et al., Characteristics and predictors of missed opportunities in lung cancer diagnosis: An electronic health record-based study. J Clin Oncol. 28:3307–3315, 2010.
Gould, M.K., Delays in lung cancer care: Time to improve. J Thorac Oncol. 4:1303–1304, 2009.
Faris, N., Yu, X., Sareen, S., et al., Preoperative evaluation of lung cancer in a community health care setting. Ann Thorac Surg. 100(2):394–400, 2015.
Nadpara, P., Madhavan, S.S., and Tworek, C., Guideline-concordant timely lung cancer care and prognosis among elderly patients in the United States: A population –based study. Cancer Epidemiol. 39:1136–1144, 2015.
Koo, M.M., Zhou, Y., and Lyratzopoulos, G., Delays in diagnosis and treatment of lung cancer: Lessons from US healthcare settings. Cancer Epidemiol. 39:1145–1147, 2015.
Kedia, S.K., Ward, K.D., Digney, S.A., et al., One-stop shop’: Lung cancer patients’ and caregivers’ perceptions of multidisciplinary care in a community healthcare setting. Transl Lung Cancer Res. 4:456–464, 2015.
Ju, F., Lee, H.K., Osarogiabon, R., et al., Computer process modeling of lung cancer diagnosis-to-treatment process. Transl Lung Cancer Res. 4:404–414, 2015.
Shao, X., Zhong, X., Li, J., et al., Bottleneck analysis to reduce surgical flow disruptions: Theory and application. IEEE Trans Autom Sci Eng. 12:127–139, 2015.
Li, J., and Meerkov, S.M., Production systems engineering. Springer, New York, NY, 2009.
Li, J., Throughput analysis in automotive paint shops: A case study. IEEE Trans Autom Sci Eng. 1:90–98, 2004.
Biller, S., Li, J., Marin, S.P., et al., Bottlenecks in Bernoulli serial lines with rework. IEEE Trans Autom Sci Eng. 7:208–217, 2010.
Wang, J., Li, J., Arinez, J., et al., Quality bottleneck transitions in flexible manufacturing systems with batch productions. IIE Trans. 45:190–205, 2013.
Wang, J., Li, J., Arinez, J., et al., Indicators for quality improvability and bottleneck sequence in flexible manufacturing systems with batch productions. Int J Prod Res. 50:6388–6402, 2012.
Wang, J., Quan, S., Li, J., et al., Modeling and analysis of work flow and staffing level in a computed tomography division of University of Wisconsin Medical Foundation. Health Care Manag Sci. 15:108–120, 2012.
Xie, X., Li, J., Swartz, C.H., et al., Modeling and analysis of rapid response process to improve patient safety in acute care. IEEE Trans Autom Sci Eng. 9:215–225, 2012.
Xie, X., Li, J., Swartz, C.H., et al., Improving response-time performance in acute care delivery: A systems approach. IEEE Trans Autom Sci Eng. 11:1240–1249, 2015.
Potosky, A.L., Saxman, S., Wallace, R.B., and Lynch, C.F., Population variations in the initial treatment of non-small-cell lung cancer. J Clin Oncol. 22:3261–3268, 2004.
Vinod, S.K., O’Connell, D.L., Simonella, L., et al., Gaps in optimal care for lung cancer. J Thorac Oncol. 3:871–879, 2008.
Ost, D.E., Niu, J., Elting, L.S., Buchholz, T.A., and Griordano, S.H., Quality gaps and comparative effectiveness in lung cancer staging and diagnosis. Chest. 145:331–345, 2014.
Backhus, L.M., Farjah, F., Varghese, T.K., et al., Appropriateness of imaging for lung cancer staging in a national cohort. J Clin Oncol. 32:3428–3435, 2014.
Funding Source
PCORI Grant IH-1304-6147.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
The authors have no conflicts of interest to report.
Early data presented at INFORMS Annual Meeting 2015, Philadelphia, PA, Nov. 2015.
Human and Animal Studies
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. For this type of retrospective study formal consent is not required. This article does not contain any studies with animals performed by any of the authors.
Additional information
This article is part of the Topical Collection on Systems-Level Quality Improvement
Appendix: Calculation Formulas
Appendix: Calculation Formulas
To evaluate the total process time, the following steps are followed:
-
Step 1: We decompose the complex process in Fig. 1 into a set of serial routes, each representing a possible trajectory of a patient. Then for a particular route i, the mean diagnosis time T i can be calculated as follows:
If each stage j in route i with M steps takes an average waiting time τ ij , then the mean time T i of diagnosis route i will be:
-
Step 2: We calculate the product of all probabilities going to the next test after each one in this route, denoted as p i in Fig. 2. Then we obtain the probability p i of a patient taking such a route. This will be the weight of route i.
-
Step 3: We denote p i T i as the weighted mean time. Summing up all the possible routes, we obtain the average mean time of overall diagnosis process.
Using this result, we introduce the so-called bottleneck waiting time, which is the one whose reduction will lead to the largest reduction in overall diagnosis-to-treatment time, comparing with reducing all other waiting times.
Specifically, let T(τ i -δτ i ) denote the resulting overall time when waiting time τ i is decreased by a small percentage δ (e.g., 10%). Then such a time τ i is the bottleneck waiting time if it is the smallest comparing with all other T(τ j -δτ j ), where j is different from i.
The above method views the diagnosis-to-surgery process as a complex network and assumes that both the trajectory routing probabilities and the waiting times are independent. In practice, the correlations between the probabilities and between the waiting times are difficult to measure since the next steps may not be carried out immediately or could be performed by independent providers. Note that even if the subsequent test is carried out immediately, this implies its waiting time is very short, and its impact on the overall waiting time will be insignificant or very small. Moreover, the scope of this analysis only considers the average performance in total delay time, thus we only need the mean waiting time.
Rights and permissions
About this article
Cite this article
Ju, F., Lee, H.K., Yu, X. et al. Reducing Bottlenecks to Improve the Efficiency of the Lung Cancer Care Delivery Process: A Process Engineering Modeling Approach to Patient-Centered Care. J Med Syst 42, 16 (2018). https://doi.org/10.1007/s10916-017-0873-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s10916-017-0873-6