Abstract
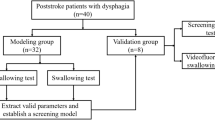
Swallowing aspiration is known as the most clinically significant symptom of swallowing disorders (dysphagia). Noninvasive methods for detection of aspiration (the entry of food into airway due to dysphagia) are of great interest as they will lead to better management of dysphagia; thus, the risk of pneumonia, length of hospital stay and overall health care expenses can be reduced. The risk of aspiration is much higher in severely dysphagic patients. Normally, aspiration is detected by an imaging technique during swallowing, which is time consuming, costly and requires the patient’s cooperation. In this study, we investigated the application of acoustical analysis of breathing and swallowing sounds for identifying patients at high risk of aspiration. We propose a novel method based on phase-space analysis of breathing sounds immediately after the swallow followed by support vector machine classification for use as a diagnostic aid for identifying patients with high risk of aspiration. We evaluated the method using breath and swallowing sounds recorded from 50 dysphagic individuals, 27 of which demonstrated silent aspiration (without cough or throat clearance) during either fiberoptic endoscopic evaluation of swallowing (FEES) or videofluoroscopic swallowing (VFS) assessment. The classification result of the proposed method was compared with those of the FEES/VFS assessment provided by speech-language pathologists; it showed 91 % sensitivity and 85 % specificity in detection of patients with severe aspiration (high risk dysphagia). The result is promising to suggest the proposed phase-space acoustical analysis method as a quick and noninvasive screening clinical tool to detect patients developing severe aspiration.





Similar content being viewed by others
References
Aboofazeli M, Moussavi Z (2005) Analysis and classification of swallowing sounds using reconstructed phase space features. In Proceedings of IEEE ICASSP
Aboofazli M, Moussavi Z (2009) Swallowing sound detection using hidden markov modeling of recurrence plot features. J Chaos, Solitons Fractals 39(2):778–783
Achem SR, Devault KR (2005) Dysphagia in aging. J Clin Gastroenterol 39(5):357–371
Ayappa I, Rapoport DM (2003) The upper airway in sleep: physiology of the pharynx. Sleep Med Rev 7(1):9–33
Beck R, Rosenhouse G, Mahagnah M, Chow R, Cugell D (2005) Measurements and theory of normal tracheal breath sounds. Ann Biomed Eng 33(10):1344–1351
Bertram C (2008) Flow-induced oscillation of collapsed tubes and airway structures. Respir Physiol Neurobiol 163(1–3):256–265
Cea L, Puertas J, Pena L (2007) Velocity measurements on highly turbulent free surface flow using ADV. Exp Fluids 42:333–348
J. E. Dempsey, F. L. Vice and J. F. Bosma (1990) Combination of cervical auscultation and video radiography in evaluation of oral and pharyngeal dysphagia [abstract], in Symposium on Dyspbagia, Johns Hopkins Hospital
Duda RO, Hart PE, Stork DG (2000) Pattern classification. Wiley, Carrollton
Goring D, Nikora V (2002) Despiking acoustic Doppler velocimeter data. J Hydraul Eng 128:117–126
Jones B (2002) Normal and abnormal swallowing: imaging in diagnosis and therapy. Springer, Berlin
Lazareck L, Moussavi Z (2004) Classification of normal and dysphagic swallowing sounds by acoustical means. IEEE Trans Biomed Eng 51(12):2013–2112
Lazarus C, Logemann JA (1987) Swallowing disorders in closed head trauma patients. Arch Phys Med Rehabil 68:79–84
Lee J, Steele CM, Chaua T (2011) Classification of healthy and abnormal swallows based on accelerometry and nasal airflow signals. Artif Intell Med 52:17–25
Lim S, Lieu PK, Phua SY, Seshadri R, Venketasub N (2001) Accuracy of bedside clinical methods compared with fiberoptic endoscopic examination of swallowing (FEES) in determining the risk of aspiration in acute stroke patients. Dysphagia 16(1):1–6
Logeman JA (1998) Evaluation and treatment of swallowing disorder. Pro-Ed, Austin
Luo XY, Hinton JS, Liew TT, Tan KK (2004) LES modeling of flow in a simple airway model. Med Eng Phy 26:403–413
Moussavi Z (2005) Assessment of swallowing sounds’ stages with hidden markov model, in 27th IEEE EMBS conf. Proc
Panther C (2005) Development of the Frazier free water protocol. Perspectives on swallowing and swallowing disorders. Dysphagia 14(1):4–9
Ramsey D, Smithard D, Kalra L (2003) Early assessments of dysphagia and aspiration risk in acute stroke patients. Stroke 34:1252–1257
Ramsey D, Smithard D, Kalra L (2005) Silent aspiration: what do we know? Dysphagia 20(3):218–225
Ramsey DJ, Smithard DG, Kalra L (2006) Can pulse oximetry or a bedside swallowing assessment be used to detect aspiration after stroke? Stroke 37(12):2984–2988
Shirazi SS, Moussavi Z (2011) Acoustical modeling of swallowing mechanism. IEEE Trans Biomed Eng 58(1):81–87
Shirazi SS, Buchel C, Daun R, Lenton L, Moussavi ZM (2012) Detection of swallows with silent aspiration using swallowing and breath sound analysis. Med Biol Eng Comput 50(12):1261–1268
Smithard DG, O’Neill PA, Park C, Morris J, Wyatt R, England R, Martin DF (1996) Complications and outcome after acute stroke. Does dysphagia matter? Stroke 27:1200–1204
Suiter DM, Leder SB (2008) Clinical utility of the 3-ounce water swallow test. Dysphagia 23(3):244–250
Zenner PM, Losinski DS, Mills RH (1995) Using cervical auscultation in the clinical dysphagia examination in long-term care. Dysphagia 10(1):27–31
Acknowledgments
The authors would like to acknowledge invaluable help of all speech-language pathologists at DeerLodge Health Center and Riverview Health Centre for recruiting dysphagic patients and collecting data.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sarraf Shirazi, S., Birjandi, A.H. & Moussavi, Z. Noninvasive and automatic diagnosis of patients at high risk of swallowing aspiration. Med Biol Eng Comput 52, 459–465 (2014). https://doi.org/10.1007/s11517-014-1151-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-014-1151-0