Abstract
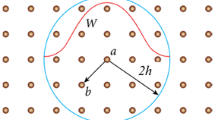
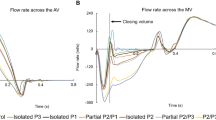
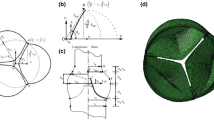
As the alternative treatment for heart failure, left ventricular assist devices (LVADs) have been widely applied to clinical practice. However, the effects of the support modes of LVADs on the biomechanical states of the aortic valve are still poorly understood. Hence, the present study investigates such effects and proposes a novel fluid–structure interaction (FSI) approach that combines the lattice Boltzmann method (LBM) and finite element (FE) method. Two support modes of LVADs, namely constant speed mode and constant flow mode, which have been widely applied to clinical practice, are also designed. Results demonstrate that the support modes of LVADs could significantly affect the biomechanical states of the aortic valve and the blood flow pattern of the ascending aorta. Compared with those in the constant flow mode, the leaflets in the constant speed mode could achieve better dynamic performance and lower stress during the systolic phase. The max radial displacement of the leaflets in the constant speed mode is at 8 mm, whereas that in the constant flow mode is at 0.8 mm. Furthermore, the outflow of LVADs directly impacts the aortic surfaces of the leaflets during the diastolic phase by increasing the level of wall shear stress of the leaflets. The leaflets in the constant speed mode receive less impact than those in the constant flow mode. The condition with such minimal impact is conducive to maintaining the normal structure of leaflets and benefits the reduction of the risk of valvular diseases. In sum, the support modes of LVADs exert a crucial effect on the biomechanical environment of the aortic valve. The constant speed mode is better than the constant flow mode in terms of providing a good hemodynamic environment for the aortic valve.








Similar content being viewed by others
References
Loebe M, Soltro E, Thohan V et al (2003) New surgical therapies for heart failure. Curr Opin Cardiol 18(3):194–198
Han J, Trumble DR (2019) Cardiac assist devices: early concepts, current technologies, and future innovations. Bioengineering (Basel) 6(1):15
Xuan YJ, Chang Y, Gu K, Gao B (2012) Hemodynamic simulation study of a novel intra-aorta left ventricular assist device. ASAIO J 58(5):462–469
Caruso MV, Gramigna V, Rossi M et al (2015) A computational fluid dynamics comparison between different outflow graft anastomosis locations of left ventricular assist device (LVAD) in a patient-specific aortic model. Int J Numer Method Biomed Eng 31(2):e02700
Aliseda A, Chivukula VK, Mcgah P, Prisco AR, Beckman JA, Garcia GJ, Mokadam NA, Mahr C (2017) LVAD outflow graft angle and thrombosis risk. ASAIO J 63(1):14–23
Zhang Q, Gao B, Chang Y (2017) Computational analysis of intra-ventricular flow pattern under partial and full support of BJUT-II VAD. Med Sci Monit 23:1043–1054
Liao S, Neidlin M, Li Z, Simpson B, Gregory SD (2018) Ventricular flow dynamics with varying LVAD inflow cannula lengths: In-silico evaluation in a multiscale model. J Biomech 72:106–115
Iizuka K, Nishinaka T, Ichihara Y, Miyamoto T, Yamazaki K (2018) Outflow graft anastomosis site design could be correlated to aortic valve regurgitation under left ventricular assist device support. J Artif Organs 21(2):150–155
Gregory SD, Stevens MC, Wu E, Fraser JF, Timms D (2013) In vitro evaluation of aortic insufficiency with a rotary left ventricular assist device. Artif Organs 37(9):802–809
Song Z, Gu K, Gao B, Wan F, Chang Y, Zeng Y (2014) Hemodynamic effects of various support modes of continuous flow LVADs on the cardiovascular system: a numerical study. Med Sci Monit 20:733–741
Grosman-Rimon L, Billia F, Kobulnik J, Pollock Bar-Ziv S, Cherney DZ, Rao V (2018) The physiological rationale for incorporating pulsatility in continuous-flow left ventricular assist devices. Cardiol Rev 26(6):294–301
Zakerzadeh R, Hsu MC, Sacks MS (2017) Computational methods for the aortic heart valve and its replacements. Expert Rev Med Dev 14(11):849–866
Zhang Q, Gao B, Yu C (2018) The effects of left ventricular assist device support level on the biomechanical states of aortic valve. Med Sci Monit 24:2003–2017
Hellmeier F, Nordmeyer S, Yevtushenko P, Bruening J, Berger F, Kuehne T, Goubergrits L, Kelm M (2018) Hemodynamic evaluation of a biological and mechanical aortic valve prosthesis using patient-specific MRI-based CFD. Artif Organs 42(1):49–57
Mendez V, Di Giuseppe M, Pasta S (2018) Comparison of hemodynamic and structural indices of ascending thoracic aortic aneurysm as predicted by 2-way FSI, CFD rigid wall simulation and patient-specific displacement-based FEA. Comput Biol Med 100:221–229
Marom G (2015) Numerical methods for fluid–structure interaction models of aortic valves. Arch Comput Methods Eng 22(4):595–620
Chandra S, Rajamannan NM, Sucosky P (2012) Computational assessment of bicuspid aortic valve wall-shear stress: implications for calcific aortic valve disease. Biomech Model Mechanobiol 11(7):1085–1096
Ghosh R, Marom G, Rotman O et al (2018) Comparative fluid-structure interaction analysis of polymeric transcatheter and surgical aortic valves’ hemodynamics and structural mechanics. J Biomech Eng. https://doi.org/10.1115/1.4040600
Halevi R, Hamdan A, Marom G et al (2016) Fluid-structure interaction modeling of calcific aortic valve disease using patient-specific three-dimensional calcification scans. Med Biol Eng Comput 54(11):1683–1694
Piatti F, Sturla F, Marom G, Sheriff J, Claiborne TE, Slepian MJ, Redaelli A, Bluestein D (2015) Hemodynamic and thrombogenic analysis of a trileaflet polymeric valve using a fluid-structure interaction approach. J Biomech 48(13):3641–3649
Wald S, Liberzon A, Avrahami I (2018) A numerical study of the hemodynamic effect of the aortic valve on coronary flow. Biomech Model Mechanobiol 17(2):319–338
Fedele M, Faggiano E, Dedè L, Quarteroni A (2017) A patient-specific aortic valve model based on moving resistive immersed implicit surfaces. Biomech Model Mechanobiol 16(5):1779–1803
Marom G, Haj-Ali R, Raanani E, Schäfers HJ, Rosenfeld M (2012) A fluid-structure interaction model of the aortic valve with coaptation and compliant aortic root. Med Biol Eng Comput 50(2):173–182
Men Y, Lai Y, Dong S et al (2017) Research on CO dispersion of a vehicular exhaust plume using Lattice Boltzmann Method and Large Eddy Simulation. Transp Res D 52:202–214
Feiger B, Vardhan M, Gounley J et al (2019) Suitability of lattice Boltzmann inlet and outlet boundary conditions for simulating flow in imagederived vasculature. Int J Numer Method Biomed Eng 35(6):e3198
Jain K, Jiang J, Strother C, Mardal KA (2016) Transitional hemodynamics in intracranial aneurysms - comparative velocity investigations with high resolution lattice Boltzmann simulations, normal resolution ANSYS simulations, and MR imaging. Med Phys 43(11):6186
Kang X, Ji Y, Liu D et al (2008) Three-dimensional lattice Boltzmann method simulating blood flow in aortic arch. Chin Phys B 17:1041–1049
Stahl B, Chopard B, Latt J (2010) Measurements of wall shear stress with the lattice Boltzmann method and staircase approximation of boundaries. Comput Fluids 39:1625–1633
Mao W, Li K, Sun W (2016) Fluid-structure interaction study of transcatheter aortic valve dynamics using smoothed particle hydrodynamics. Cardiovasc Eng Technol 7(4):374–388
Boccadifuoco A, Mariotti A, Capellini K et al (2018) Validation of numerical simulations of thoracic aorta hemodynamics: comparison with in vivo measurements and stochastic sensitivity analysis. Cardiovasc Eng Technol 9(4):688–706
Pauls JP, Stevens MC, Bartnikowski N, Fraser JF, Gregory SD, Tansley G (2016) Evaluation of physiological control systems for rotary left ventricular assist devices: an in-vitro study. Ann Biomed Eng 44(8):2377–2387
SIMULIA SIMULIA XFlow 2018 User Guide. Dassault Systemes Simulia Corp. RI, Providence, p 2018
Mei S, de Souza Júnior FSN, Kuan MYS, Green NC, Espino DM (2016) Hemodynamics through the congenitally bicuspid aortic valve: a computational fluid dynamics comparison of opening orifice area and leaflet orientation. Perfusion 31(8):683–690
Kemp I, Dellimore K, Rodriguez R, Scheffer C, Blaine D, Weich H, Doubell A (2013) Experimental validation of the fluid-structure interaction simulation of a bioprosthetic aortic heart valve. Australas Phys Eng Sci Med 36(3):363–373
Jorde UP, Uriel N, Nahumi N, Bejar D, Gonzalez-Costello J, Thomas SS, Han J, Morrison KA, Jones S, Kodali S, Hahn RT, Shames S, Yuzefpolskaya M, Colombo P, Takayama H, Naka Y (2014) Prevalence, significance, and management of aortic insufficiency in continuous flow left ventricular assist device recipients. Circ Heart Fail 7(2):310–319
Gasparovic H, Kopjar T, Saeed D, Cikes M, Svetina L, Petricevic M, Lovric D, Milicic D, Biocina B (2017) De novo aortic regurgitation after continuous-flow left ventricular assist device implantation. Ann Thorac Surg 104(2):704–711
Stephens EH, Han J, Trawick EA, di Martino ES, Akkiraju H, Brown LM, Connell JP, Grande-Allen KJ, Vunjak-Novakovic G, Takayama H (2018) Left-ventricular assist device impact on aortic valve mechanics, proteomics and ultrastructure. Ann Thorac Surg 105(2):572–580
Truby LK, Garan AR, Givens RC et al (2018) Aortic insufficiency during contemporary left ventricular assist device support: analysis of the INTERMACS registry. JACC Heart Fail 6(11):951–960
Aggarwal A, Raghuvir R, Eryazici P, Macaluso G, Sharma P, Blair C, Tatooles AJ, Pappas PS, Bhat G (2013) The development of aortic insufficiency in continuous-flow left ventricular assist device-supported patients. Ann Thorac Surg 95(2):493–498
Sugiura T, Kurihara C, Kawabori M et al (2019) Concomitant valve procedures in patients undergoing continuous-flow left ventricular assist device implantation: A single-center experience. J Thorac Cardiovasc Surg 158(4):1083–1089
Selmi M, Chiu WC, Chivukula VK, Melisurgo G, Beckman JA, Mahr C, Aliseda A, Votta E, Redaelli A, Slepian MJ, Bluestein D, Pappalardo F, Consolo F (2019) Blood damage in left ventricular assist devices: pump thrombosis or system thrombosis? Int J Artif Organs 42(3):113–124
Mao W, Li K, Sun W et al (2016) Fluid-structure interaction study of transcatheter aortic valve dynamics using smoothed particle hydrodynamics. Cardiovasc Eng Technol 7(4):374–388
Wang TS, Hernandez AF, Felker GM et al (2014) Valvular heart disease in patients supported with left ventricular assist devices. Circ Heart Fail 7(1):215–222
Marcucci L, Washio T, Yanagida T (2019) Proposed mechanism for the length dependence of the force developed in maximally activated muscles. Sci Rep 9(1):1317
Cowger J, Pagani FD, Haft JW et al (2010) The development of aortic insufficiency in left ventricular assist device-supported patients. Circ Heart Fail 3:668–674
Hatano M, Kinugawa K, Shiga T, Kato N, Endo M, Hisagi M, Nishimura T, Yao A, Hirata Y, Kyo S, Ono M, Nagai R (2011) Less frequent opening of the aortic valve and a continuous flow pump are risk factors for postoperative onset of aortic insufficiency in patients with a left ventricular assist device. Circ J 75:1147–1155
Mudd JO, Cuda JD, Halushka M et al (2008) Fusion of aortic valve commissures in patients supported by a continuous axial flow left ventricular assist device. J Heart Lung Transplant 27:1269–1274
Joda A, Jin Z, Haverich A, Summers J, Korossis S (2016) Multiphysics simulation of the effect of leaflet thickness inhomogeneity and material anisotropy on the stress-strain distribution on the aortic valve. J Biomech 49(12):2502–2512
Gao B, Chang Y, Gu K, Zeng Y, Liu Y (2012) A pulsatile control algorithm of continuous-flow pump for heart recovery. ASAIO J 58(4):343–352
Naito N, Nishimura T, Iizuka K, Takewa Y, Umeki A, Ando M, Ono M, Tatsumi E (2018) Rotational speed modulation used with continuous-flow left ventricular assist device provides good pulsatility. Interact Cardiovasc Thorac Surg 26(1):119–123
Gao B, Chang Y, Xuan Y, Zeng Y, Liu Y (2013) The hemodynamic effect of the support mode for the intra-aorta pump on the cardiovascular system. Artif Organs 37(2):157–165
Funding
This study was partly funded by the National Natural Science Foundation of China (Grant Nos. 11602007, 11572014, 61931013, and 11832003), the Key Research and Development Program (2016YFC0103201, 2017YFC0111104), and New Talent (015000514118002).
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gao, B., Zhang, Q. & Chang, Y. Hemodynamic effects of support modes of LVADs on the aortic valve. Med Biol Eng Comput 57, 2657–2671 (2019). https://doi.org/10.1007/s11517-019-02058-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-019-02058-y