Abstract
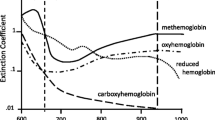
The oxyhemoglobin dissociation curve describes the relationship between the partial pressure of oxygen and the percent of hemoglobin saturated with oxygen and varies with chemical and physical factors that differ for every patient. If variability could be determined, patient-specific oxygen therapy could be administered. We have developed a procedure for characterizing variations in the oxygen dissociation curve. The purpose of this study was to validate this procedure in surgical patients. The procedure uses an automated system to alter oxygen therapy during surgery, within safe operational levels, and fit to Hill’s equation non-invasive measurements of end-tidal oxygen and peripheral pulse oxygen saturation. The best-fit parameters for the Hill equation, estimated by iterative least squares, provide an apparent dissociation curve, meaningful of the patient-specific pulse oximeter response. Thirty-nine patients participated in this study. Using patient-specific parameter values increases correlation when compared with standard values. The procedure improved the model fit of patient saturation values significantly in 19 patients. This paper has demonstrated a procedure for determining patient-specific pulse oximeter response. This procedure determined best-fit parameters resulting in a significantly improved fit when compared with standard values. These best-fit parameters increased the coefficient of determination R2 in all cases.

This patient-specific procedure improves fit significantly compared to standard estimates




Similar content being viewed by others
References
Applegate RL II, Dorotta IL, Wells B, Juma D, Applegate PM (2016) The relationship between oxygen reserve index and arterial partial pressure of oxygen during surgery. Anesthesia and Analgesia 123(3):626
Averick BM, Carter RG, Xue GL, More J (1992) The minpack-2 test problem collection. Tech. rep., Argonne National Lab., IL (United States)
Berg JM, Tymoczko JL, Stryer L (2002) Hemoglobin transports oxygen efficiently by binding oxygen cooperatively. WH Freeman & Co, New York
Brockway J, Hay WW Jr (1998) Prediction of arterial partial pressure of oxygen with pulse oxygen saturation measurements. The Journal of Pediatrics 133(1):63–66
Buerk DG, Bridges EW (1986) A simplified algorithm for computing the variation in oxyhemoglobin saturation with ph, pco2, t and dpg. Chem Eng Commun 47(1-3):113–124
Burk KM, Kuck K, Orr JA Evaluation and application of a method for estimating nasal end-tidal o 2 fraction while administering supplemental o 2. Journal of Clinical Monitoring and Computing: 1–10
Burk KM, Sakata DJ, Kuck K, Orr JA (2019) Comparing nasal end-tidal carbon dioxide measurement variation and agreement while delivering pulsed and continuous flow oxygen in volunteers and patients. Anesthesia and Analgesia
Collins JA, Rudenski A, Gibson J, Howard L, O’Driscoll R (2015) Relating oxygen partial pressure, saturation and content: the haemoglobin–oxygen dissociation curve. Breathe 11(3):194– 201
Dash RK, Korman B, Bassingthwaighte JB (2016) Simple accurate mathematical models of blood hbo2 and hbco2 dissociation curves at varied physiological conditions: evaluation and comparison with other models. Eur J Appl Physiol 116(1):97–113
Donders W, Huberts W, van de Vosse F, Delhaas T (2015) Personalization of models with many model parameters: an efficient sensitivity analysis approach. Int J Numer Method Biomed Eng 31(10)
Downs JS (1994) Prevention of hypoxemia: the simple, logical, but incorrect solution. J Clin Anesth 6 (3):180–181
Dubreuil S, Berveiller M, Petitjean F, Salaün M (2014) Construction of bootstrap confidence intervals on sensitivity indices computed by polynomial chaos expansion. Reliab Eng Syst Safe 121:263–275
Farmery A, Roe P (1996) A model to describe the rate of oxyhaemoglobin desaturation during apnoea. Br J Anaesth 76(2):284–291
Fu ES, Downs JB, Schweiger JW, Miguel RV, Smith RA (2004) Supplemental oxygen impairs detection of hypoventilation by pulse oximetry. Chest 126(5):1552–1558
Gomez-Cambronero J (2001) The oxygen dissociation curve of hemoglobin: bridging the gap between biochemistry and physiology. J Chem Educ 78(6):757
Hardman JG, Wills JS, Aitkenhead AR (2000) Factors determining the onset and course of hypoxemia during apnea: an investigation using physiological modelling. Anesthesia & Analgesia 90(3):619–624
Hay WW, Brockway JM, Eyzaguirre M (1989) Neonatal pulse oximetry: accuracy and reliability. Pediatrics 83(5):717–722
Heitman SJ, Atkar RS, Hajduk EA, Wanner RA, Flemons WW (2002) Validation of nasal pressure for the identification of apneas/hypopneas during sleep. American Journal of Respiratory and Critical Care Medicine 166(3):386–391
Hemmings HC, Hopkins PM (2006) Foundations of anesthesia: basic sciences for clinical practice. Elsevier Health Sciences
Hsia CC (1998) Respiratory function of hemoglobin. New England J Med 338(4):239–248
Jones E, Oliphant T, Peterson P, et al. (2001) SciPy: open source scientific tools for Python. http://www.scipy.org/. Online: Accessed 01/01/2019
Keidan I, Gravenstein D, Berkenstadt H, Ziv A, Shavit I, Sidi A (2008) Supplemental oxygen compromises the use of pulse oximetry for detection of apnea and hypoventilation during sedation in simulated pediatric patients. Pediatrics 122(2):293–298
Leow MKS (2007) Configuration of the hemoglobin oxygen dissociation curve demystified: a basic mathematical proof for medical and biological sciences undergraduates. Advances in Physiology Education 31(2):198–201
Myles P, Heap M, Langley M (1993) Agreement between end-tidal oxygen concentration and the alveolar gas equation: pre and post cardiopulmonary bypass. Anaesth Intensive Care 21:240–1
Næraa N, Boye E (1962) The influence of simultaneous, independent changes in ph and carbon dioxide tension on the in-vitro oxygen tension-saturation relationship of human whole blood. Acta Anaesthesiol Scand 6:20–20
Severinghaus J (1958) Oxyhemoglobin dissociation curve correction for temperature and ph variation in human blood. J Appl Physiol 12(3):485–486
Siggaard-Andersen O, Salling N (1971) Oxygen-linked hydrogen ion binding of human hemoglobin. effects of carbon dioxide and 2, 3-diphosphoglycerate. ii. studies on whole blood. Scandinavian Journal of Clinical and Laboratory Investigation 27(4):361–366
Siggaard-Andersen O, Wimberley P, Göthgen I, Siggaard-Andersen M (1984) A mathematical model of the hemoglobin-oxygen dissociation curve of human blood and of the oxygen partial pressure as a function of temperature. Clin Chem 30(10):1646–1651
Thurnheer R, Xie X, Bloch KE (2001) Accuracy of nasal cannula pressure recordings for assessment of ventilation during sleep. American Journal of Respiratory and Critical Care Medicine 164(10):1914–1919
Funding
This work was financially supported by a Utah Space Grant Consortium Graduate Research Fellowship (K.M.B.) and was partially funded by Dynasthetics, LLC.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Kyle Burk: Dynasthetics, LLC and Joseph Orr: Dynasthetics, LLC
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable standards.
Informed consent was obtained from all individual participants included in the study.
This article does not contain any studies with animals performed by any of the authors.
Rights and permissions
About this article
Cite this article
Burk, K.M., Orr, J.A. A procedure for determining subject-specific pulse oxygen saturation response. Med Biol Eng Comput 58, 753–761 (2020). https://doi.org/10.1007/s11517-019-02105-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-019-02105-8