Abstract
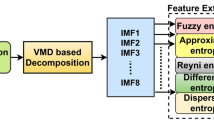
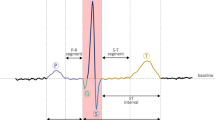
Neurally mediated syncope (NMS) is the most common type of syncope, and head up tilt test (HUTT) is, so far, the most appropriate tool to identify NMS. In this work, an effort to predict the NMS before performing the HUTT is attempted. To achieve this, the heart rate variability (HRV) at rest and during the first minutes of tilting position during HUTT was analyzed using both time and frequency domains. Various features from HRV regularity and complexity, along with wavelet higher-order spectrum (WHOS) analysis in low-frequency (LF) and high-frequency (HF) bands were examined. The experimental results from 26 patients with history of NMS have shown that at rest, a time domain entropy measure and WHOS-based features in LF band exhibit significant differences between positive and negative HUTT as well as among 10 healthy subjects and NMS patients. The best performance of multilayer perceptron neural network (MPNN) was achieved by using an input vector consisted of WHOS-based HRV features in the LF zone and systolic blood pressure from the resting period, yielding an accuracy of 89.7%, assessed by 5-fold cross-validation. The promising results presented here pave the way for an early prediction of the HUTT outcome from resting state, contributing to the identification of patients at higher risk NMS.

The HRV analysis along with systolic blood pressure at rest predict NMS using a multilayer perceptron neural network.


Similar content being viewed by others
References
Addison PS (2005) Wavelet transforms and the ECG: a review. Physiol Meas 26(5):R155
Addison PS (2017) The illustrated wavelet transform handbook: introductory theory and applications in science, engineering, medicine and finance. CRC Press
Akizuki H, Hashiguchi N (2019) Heart rate variability in patients presenting with neurally mediated syncope in an emergency department. Amer J Emerg Med
Bandt C, Pompe B (2002) Permutation entropy: a natural complexity measure for time series. Phys Rev Lett 88(17):174102
Bari V, Marchi A, De Maria B, Rossato G, Nollo G, Faes L, Porta A (2016) Nonlinear effects of respiration on the crosstalk between cardiovascular and cerebrovascular control systems. Phil TransRoyal Soc A Math Phys Eng Sci 374(2067):20150179
Bellard E, Fortrat JO, Schang D, Dupuis JM, Victor J, Lefthériotis G (2003) Changes in the transthoracic impedance signal predict the outcome of a 70 head-up tilt test. Clin Sci 104(2):119–126
Benditt DG, Ferguson DW, Grubb BP, Kapoor WN, Kugler J, Lerman BB, Maloney JD, Ravielle A, Ross B, Sutton R et al (1996) Tilt table testing for assessing syncope. J Am Coll Cardiol 28(1):263–275
Bishop CM (1995) Neural networks for pattern recognition. Oxford University Press
Blanc JJ (2013) Clinical laboratory testing: what is the role of tilt-table testing, active standing test, carotid massage, electrophysiological testing and ATP test in the syncope evaluation? Progress Cardiovas Dis 55(4):418–424
Blendea D, McPherson CA, Pop S, Anton FP, Crisan S, Ruskin JN (2019) Isolated very low QRS voltage predicts response to tilt-table testing in patients with neurally mediated syncope. Pacing Clin Electrophys
Borovik A, Negulyaev V, Tarasova O, Kheymets G, Pevzner A, Ermishkin V, Zyuzina N, Rogoza A, Vinogradova O (2019) Disorders of synchronization of blood pressure and heart rate precede the development of vasovagal syncope during orthostasis. Hum Physiol 45(4):405–411
Brennan M, Palaniswami M, Kamen P (2001) Do existing measures of Poincare plot geometry reflect nonlinear features of heart rate variability? IEEE Trans Biomed Eng 48(11):1342–1347
Brennan M, Palaniswami M, Kamen P (2002) Poincare plot interpretation using a physiological model of HRV based on a network of oscillators. Amer J Physiol Heart Circul Physiol 283(5):H1873–H1886
Brignole M, Menozzi C, Del Rosso A, Costa S, Gaggioli G, Na Bottoni, Bartoli P, Sutton R (2000) New classification of haemodynamics of vasovagal syncope: beyond the VASIS classification: analysis of the pre-syncopal phase of the tilt test without and with nitroglycerin challenge. EP Europace 2(1): 66–76
Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martín A et al (2018) 2018 ESC guidelines for the diagnosis and management of syncope. European Heart J 39(21):1883–1948
Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A, Fedorowski A, Furlan R, Kenny RA, Martín A et al (2018) Practical instructions for the 2018 ESC guidelines for the diagnosis and management of syncope. European Heart J 39(21):e43–e80
Ciliberti MAP, Santoro F, Di Martino LFM, Rinaldi AC, Salvemini G, Cipriani F, Triggiani AI, Moscatelli F, Valenzano A, Di Biase M et al (2017) Predictive value of very low frequency at spectral analysis among patients with unexplained syncope assessed by head-up tilt testing. Arch Cardiovas Dis
Colman N, Nahm K, Ganzeboom K, Shen WK, Reitsma J, Linzer M, Wieling W, Kaufmann H (2004) Epidemiology of reflex syncope. Clin Auton Res 14(1):i9–i17
Couceiro R, Carvalho P, Paiva RP, Muehlsteff J, Henriques J, Eickholt C, Brinkmeyer C, Kelm M, Meyer C (2015) Real-time prediction of neurally mediated syncope. IEEE J Biomed Health Inform 20(2):508–520
Faes L, Widesott L, Del Greco M, Antolini R, Nollo G (2005) Causal cross-spectral analysis of heart rate and blood pressure variability for describing the impairment of the cardiovascular control in neurally mediated syncope. IEEE Trans Biomed Eng 53(1):65–73
Faes L, Nollo G, Porta A (2013) Mechanisms of causal interaction between short-term RR interval and systolic arterial pressure oscillations during orthostatic challenge. J App Physiol 114(12):1657–1667
Folino AF, Russo G, Porta A, Buja G, Cerutti S, Iliceto S (2007) Modulations of autonomic activity leading to tilt-mediated syncope. Int J Cardiol 120(1):102–107
Goldberger AL, Amaral LA, Glass L, Hausdorff JM, Ivanov PC, Mark RG, Mietus JE, Moody GB, Peng CK, Stanley HE (2000) Physiobank, Physiotoolkit, and Physionet: components of a new research resource for complex physiologic signals. Circulation 101(23):e215–e220
Graff B, Graff G, Makowiec D, Kaczkowska A, Wejer D, Budrejko S, Kozłowski D, Narkiewicz K (2015) Entropy measures in the assessment of heart rate variability in patients with cardiodepressive vasovagal syncope. Entropy 17(3):1007–1022
Grubb BP (2005) Neurocardiogenic syncope and related disorders of orthostatic intolerance. Circulation 111(22):2997–3006
Heldt T, Oefinger M, Hoshiyama M, Mark R (2003) Circulatory response to passive and active changes in posture. In: Computers in cardiology. IEEE, pp 263–266
Itchhaporia D, Snow PB, Almassy RJ, Oetgen WJ (1996) Artificial neural networks: current status in cardiovascular medicine. J Am Coll Cardiol 28(2):515–521
Khodor N, Carrault G, Matelot D, Amoud H, Khalil M, du Boullay NT, Carre F, Hernández A (2016) Early syncope detection during head up tilt test by analyzing interactions between cardio-vascular signals. Digit Sig Process 49:86–94
Klabunde R (2011) Cardiovascular physiology concepts. Lippincott Williams & Wilkins
Kochiadakis G, Rombola A, Kanoupakis E, Simantirakis E, Chlouverakis G, Vardas P (1997) Assessment of autonomic function at rest and during tilt testing in patients with vasovagal syncope. Amer Heart J 134(3):459–466
Kohavi R (1995) A study of cross-validation and bootstamp for accuracy estimation and model selection. In: Proceedings of the 14th International Conference on Artificial Intelligence. Montreal, Canada, pp 1137–1143
Kohavi R, John GH (1997) Wrappers for feature subset selection. Artif Intell 97(1-2):273–324
Kostoglou K, Schondorf R, Benoit J, Balegh S, Mitsis GD (2018) Prediction of the time to syncope occurrence in patients diagnosed with vasovagal syncope. In: Intracranial pressure & neuromonitoring XVI. Springer, pp 313–316
Krittanawong C, Zhang H, Wang Z, Aydar M, Kitai T (2017) Artificial intelligence in precision cardiovascular medicine. J Am Coll Cardiol 69(21):2657–2664
Lippman N, Stein KM, Lerman BB (1995) Failure to decrease parasympathetic tone during upright tilt predicts a positive tilt-table test. Amer J Cardiol 75(8):591–595
Lisboa PJ (2002) A review of evidence of health benefit from artificial neural networks in medical intervention. Neural Netw 15(1):11–39
Mäkikallio TH, Seppänen T, Niemelä M, Airaksinen KJ, Tulppo M, Huikuri HV (1996) Abnormalities in beat to beat complexity of heart rate dynamics in patients with a previous myocardial infarction. J Am Coll Cardiol 28(4):1005–1011
Makowiec D, Graff B, Struzik ZR (2017) Multistructure index characterization of heart rate and systolic blood pressure reveals precursory signs of syncope. Scient Rep 7(1):419
Malik M, Bigger JT, Camm AJ, Kleiger RE, Malliani A, Moss AJ, Schwartz PJ (1996) Heart rate variability. Eur Heart J 17(3):354–381
McGraw KO, Wong SP (1992) A common language effect size statistic. Psychol Bull 111 (2):361
Méndez-Magdaleno LE, Dorantes-Méndez G, Charleston-Villalobos S, Aljama-Corrales T (2019) Nonlinear, time-varying and frequency-selective analysis during the orthostatic challenge in patients with vasovagal syncope. In: Latin American Conference on Biomedical Engineering. Springer, pp 113–120
Mitchell TM et al (1997) Machine learning. WCB
Morillo CA, Klein GJ, Jones DL, Yee R (1994) Time and frequency domain analyses of heart rate variability during orthostatic stress in patients with neurally mediated syncope. Amer J Cardiol 74 (12):1258–1262
Mosqueda-Garcia R, Furlan R, Fernandez-Violante R, Desai T, Snell M, Jarai Z, Ananthram V, Robertson RM, Robertson D et al (1997) Sympathetic and baroreceptor reflex function in neurally mediated syncope evoked by tilt. J Clin Invest 99(11):2736–2744
Mosqueda-Garcia R, Furlan R, Tank J, Fernandez-Violante R (2000) The elusive pathophysiology of neurally mediated syncope. Circulation 102(23):2898–2906
Moya A, Sutton R, Ammirati F, Blanc JJ, Brignole M, Dahm JB, Deharo JC, Gajek J, Gjesdal K, Krahn A et al (2009) Guidelines for the diagnosis and management of syncope (version 2009). European Heart J 30(21):2631–2671
Nadi AK (1998) Higher-order statistics in signal processing. Cambridge University Press, Cambridge, U.K
Nikias C, Petropolu A (1993) Higher-order spectra analysis: a nonlinear signal processing framework. PTR Prentice-Hall Inc, New Jersey, NJ
Ocon AJ, Medow MS, Taneja I, Stewart JM (2011) Respiration drives phase synchronization between blood pressure and RR interval following loss of cardiovagal baroreflex during vasovagal syncope. Amer J Physiol Heart Circul Physiol 300(2):H527–H540
Pan J, Tompkins WJ (1985) A real-time QRS detection algorithm. IEEE Trans Biomed Eng BME 32(3):230–236
Pincus SM, Gladstone IM, Ehrenkranz RA (1991) A regularity statistic for medical data analysis. J Clin Monit Comput 7(4):335–345
Porta A, Guzzetti S, Montano N, Furlan R, Pagani M, Malliani A, Cerutti S (2001) Entropy, entropy rate, and pattern classification as tools to typify complexity in short heart period variability series. IEEE Trans Biomed Eng 48(11):1282–1291
Pruvot E, Vesin J, Schlaepfer J, Eromer M, Kappenberger L (1994) Autonomic imbalance assessed by heart rate variability analysis in vasovagal syncope. Pacing Clin Electrophysiol 17(11):2201–2206
Richman JS, Moorman JR (2000) Physiological time-series analysis using approximate entropy and sample entropy. Amer J Physiol Heart Circul Physiol 278(6):H2039–H2049
Riedl M, Müller A, Wessel N (2013) Practical considerations of permutation entropy. Eur Phys J Spec Top 222(2):249–262
Schang D, Feuilloy M, Plantier G, Fortrat JO, Nicolas P (2006) Early prediction of unexplained syncope by support vector machines. Physiol Meas 28(2):185
Schlenker J, Socha V, Riedlbauchová L, Nedělka T, Schlenker A, Potočková V, Malá Š, Kutílek P (2016) Recurrence plot of heart rate variability signal in patients with vasovagal syncopes. Biomed Sig Process Control 25:1–11
Sheela KG, Deepa SN (2013) Review on methods to fix number of hidden neurons in neural networks. Math Probl Eng 2013
Soteriades ES, Evans JC, Larson MG, Chen MH, Chen L, Benjamin EJ, Levy D (2002) Incidence and prognosis of syncope. N Engl J Med 347(12):878–885
Taplidou A, Hadjileontiadis LJ (2010) Analysis of wheezes using wavelet higher order spectral features. IEEE Trans Biomed Eng 57(7):1596–1610
Virag N, Erickson M, Taraborrelli P, Vetter R, Lim PB, Sutton R (2018) Predicting vasovagal syncope from heart rate and blood pressure: a prospective study in 140 subjects. Heart Rhythm 15 (9):1404–1410
Jamšek J, Stefanovska A, McClintock PVE (2007) Wavelet bispectral analysis for the study of interactions among oscillators whose basic frequencies are significantly time variable. Phys Rev E 76:046221
Zyśko D, Fedorowski A, Sutton R (2016) Cardiac arrest during recovery after tilt-induced vasodepressor syncope in a 76-year old man. J Acute Med 6(3):67–69
Acknowledgements
The authors would like to thank the patients that voluntary participated in the HUTT and provided their data for the current research work. They also want to thank the medical and nursing staff of the Third Cardiology Department, Hippocration Hospital for the excellent cooperation. The authors are also grateful to Mr. A. Fotoglidis for his assistance in data collection and to Dr. A. Antoniadis for his valuable suggestions and comments on the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
The study protocol was approved by the Bioethics Committee of Medical School of Aristotle University of Thessaloniki, Greece. All patients provided a written consent for their voluntary participation in the HUTT and use of their data for research purposes, after granting the privacy of their personal information. Subjects held the right to withdraw from the procedure at any time, without providing any justification. Recruitment and study procedures were carried out according to institutional and international guidelines on research involving adult human beings.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Appendix A
1.1 A.1 Wavelet higher-order spectral analysis
-
1)
The continuous wavelet transform (CWT) is defined as [2]
$$ \begin{array}{@{}rcl@{}} W_{x}(a,b)=\frac{1}{\sqrt{a}}{\int}_{-\infty}^{+\infty}x(t)\psi^{*}\left( \frac{t-b}{a}\right)dt, \end{array} $$(A1)where x(t) is the signal in time domain, * is the complex conjugate, and ψ(t) is the mother wavelet scaled by a factor α, α > 0 and dilated by a factor b.
-
2)
The bispectrum is defined as [48]
$$ \begin{array}{@{}rcl@{}} B(\omega_{1} , \omega_{2}) = E \lbrace X_{i}(\omega_{1}) X_{i}(\omega_{2}) X_{i}^{*}(\omega_{1} + \omega_{2})\rbrace, \end{array} $$(A2)where X(ωi),i = 1,2, is the complex Fourier coefficient of the process {x(k)} at frequencies ωi and X∗(ωi) is its complex conjugate [47].
-
3)
The wavelet bispectrum is defined as [62]
$$ WB_{x}(a_{1},a_{2})={\int}_{T}W_{x}^{*}(a,\tau) W_{x}(a_{1},\tau) W_{x}(a_{2},\tau)d\tau, $$(A3)where the integration is done over a finite time interval T : τ0 ≤ τ ≤ τ1 and α, α1,α2 satisfy the subsequent rule:
$$ \begin{array}{@{}rcl@{}} \frac{1}{a}=\frac{1}{a_{1}}+ \frac{1}{a_{2}}. \end{array} $$(A4) -
4)
The instantaneous wavelet bispectrum IWBS can be defined as a time dependent complex quantity and is defined as [62]
IWBx(a1,a2,t)
$$ \begin{array}{@{}rcl@{}} =|{IWB_{x}(a_{1},a_{2},t)}|e^{j\angle IWB_{x}(a_{1},a_{2},t)}=A_{x} e^{j \varphi_{x}}. \end{array} $$(A5) -
5)
The instantaneous wavelet biamplitude WBSAmp from which it is possible to infer the relative strength of the interaction given by [62]
$$ \begin{array}{@{}rcl@{}} A_{x}(a_{1},a_{2},t)=|{IWB_{x}(a_{1},a_{2},t)}|. \end{array} $$(A6) -
6)
The maximum instantaneous wavelet biamplitude of the local peaks (LP) in the time interval t is defined as [60]
$$ A_{x}^{{LP_{i}}}(\omega_{c_{1}} ,\omega_{c_{2}},t)=A_{x}^{{LP_{i}}}(\omega_{1} , \omega_{2},t)|_{A_{x}^{{LP_{i}}}(\omega_{1} , \omega_{2})=max}, $$(A7)and \(c^{i}_{LP}=(\omega _{c_{1}} ,\omega _{c_{2}},t)^{i}, i=1,2,....,n\) is the position where peak i has its maximum value and n is the number of LP of each time interval.
Appendix B
1.1 B.1 Multilayer perceptron neural network (MPNN)
Multilayer perceptron neural networks (MPNNs) are feed-forward artificial neural networks with applications in pattern recognition and classification. The architecture of MPNN consists of three sequential layers: input, one or more hidden, and output layer. The input layer receives outward inputs and the hidden layer through neurons executes processing and transmission of the input information to the output, which the last produces the classification results. The neural network model is described from a nonlinear function with a set of input variables xi and a set of output variables yk, controlled by a vector w of adjustable parameters. The overall network function is [8]:
where \(w_{ji}^{(1)}, w_{j0}^{(1)}\) are weights and bias similarly in the 1st layer, h(⋅) a differentiable nonlinear activation function, \(w_{kj}^{(2)}, w_{k0}^{(2)}\) weights and bias in the 2nd layer, and \(\sigma (a)=\frac {1}{1+e^{-a}}\) a sigmoid activation function for binary classification.
The information is sent alternately forwards and backwards through the network and this procedure is known as error back-propagation, which describes the training of MLP using gradient descent applied to a sum-of-squares error function [8]:
where a training set comprising a set of input vectors {xn},n = 1,...,N, together with a set of target vectors {tn}. An iterative procedure for minimization of an error function is used through training algorithms to adjust the weights.
Rights and permissions
About this article
Cite this article
Myrovali, E., Fragakis, N., Vassilikos, V. et al. Efficient syncope prediction from resting state clinical data using wavelet bispectrum and multilayer perceptron neural network. Med Biol Eng Comput 59, 1311–1324 (2021). https://doi.org/10.1007/s11517-021-02353-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11517-021-02353-7