Abstract
Purpose
Accurate Transrectal Ultrasound (TRUS)-guided prostate needle biopsy requires registering preoperative 3D TRUS or MR image, in which tumors and other suspicious areas are visible, to intraoperative 2D TRUS images. Such image registration is time-consuming while its real-time implementation is yet to be developed. To bypass this registration step, robotic needle biopsy systems can be used to place the US probe at the same position relative to the prostate during the 3D and 2D image acquisition to ensure similar prostate deformation. To have such similar deformation, only visual feedback is not sufficient as such feedback can be used to only guarantee that the whole prostate is within the field of view irrespective of the probe’s orientation. As such, contact pressure feedback can be utilized to ensure consistent minimum contact between the probe and prostate.
Method
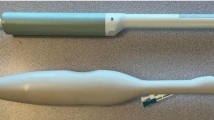
A robotic system is proposed where a TRUS probe with pressure sensor array is used. The contact pressure can be measured during imaging and used to provide feedback in conjunction with an optimization algorithm for consistent probe positioning. The robotic system is driven by the feedback to position the probe such that pressure pattern of the sensors during 2D image acquisition is similar to the pressure pattern during 3D image acquisition. The proposed method takes into account the patient’s body movement expected during image acquisition. In this study, an in silico phantom is used where the simulated contact pressure distribution required in the optimization algorithm is obtained using a prostate finite element model.
Result
Starting from an arbitrary position where the probe contacts the phantom, this position was varied systematically until a position corresponding to maximum pressure pattern similarity between contact pressure patterns corresponding to the 2D and 3D imaging was achieved successfully.
Conclusion
Results obtained from the in silico phantom study indicate that the proposed technique is capable of ensuring having only minimal relative prostate deformation between preoperative image acquisition and intraoperative imaging used for guiding needle biopsy, paving the way for faster and more accurate registration.










Similar content being viewed by others
References
Canadian Cancer Society, Prostate Cancer Statistics: www.cancer.ca. Accessed 10 January 2013
Salomon G, Kollerman J, Thederan I, Chun FKH, Budaus L, Schlomm T, Isbarn H, Heinzer H, Huland H, Graefen M (2008) Evaluation of prostate cancer detection with ultrasound real-time elastography: a comparison with step section pathological analysis after radical prostatectomy. J Eur Urol 54:1354–1362
Fung YC (1981) Biomechanical properties of living tissue. Springer, New York
Anderson WAD (1953) Pathology. C. V. Mosby Co., St. Louis
Miyanaga N, Akaza H, Yamakawa M, Oikawa T, Sekido N, Hinotsu S, Kawai K, Shimazui T, Shiina T (2006) Tissue elasticity imaging for diagnosis of prostate cancer: a preliminary report. J Urol 13(12):1514–1518
Pallwein L, Mitterberger M, Gradl J, Aigner F, Horninger W, Strasser H, Bartsch G, Zur Nedden D, Frauscher F (2007) Value of contrast-enhanced ultrasound and elastography in imaging of prostate cancer. Curr Opin Urol 17(1):39–47
Zhang Y, Tang J, Li Y, Fei X, He E, Li Q, Shi H (2012) The contribution of strain patterns in characterization of prostate peripheral zone lesions at transrectal ultrasonography. Acta Radiologica 53(1):119–126
Presti JC (2000) Prostate cancer: assessment of risk using digital rectal examination, tumour grade, prostate-specific antigen, and systematic biopsy. Radiologic Clin North Am 38(1):49–58
Loch T (2007) Urologic imaging for localized prostate cancer in 2007. World J Urol 25:121–129
Song S, Cho NB, Iordachita II, Guion P, Fichtinger G, Whitcomb LL (2011) A study of needle image article localization in confirmation imaging of MRI-guided robotic prostate biopsy. In: IEEE international conference on robotics and automation
Boris A, Hadaschik BA, Kuru TH, Tulea C, Rieker P, Popeneciu IV, Simpfendörfer T, Huber J, Zogal P, Teber D, Pahernik S, Roethke M, Zamecnik P, Roth W, Sakas G, Schlemmer HP, Hohenfellner MA (2011) Novel stereotactic prostate biopsy system integrating pre-interventional magnetic resonance imaging and live ultrasound fusion. JURO 186(6):2214–2220
De Silva T, Bax J, Fenster A, Samarabandu J, Ward AD (2011) Quantification of prostate deformation due to needle insertion during TRUS-guided biopsy: comparison of hand-held and mechanically stabilized systems. In: SPIE Proceedings
Reynier C, Troccaz J, Fourneret P, Dusserre A, Gay-Jeune C, Descotes J, Bolla M, Giraud J (2004) MRI/TRUS data fusion for prostate brachytherapy. Preliminary results. Med Phys 31:1568–1575
Wei Z, Wan G, Gardi L, Mills G, Downey D, Fenster A (2004) Robot-assisted 3D-TRUS guided prostate brachytherapy: system integration and validation. Med Phys 31(3):539–548
Pieper S, Halle M, Kikinis R (2004) 3D SLICER. In: Proceedings of the 1st IEEE international symposium on biomedical imaging: from nano to Macro, pp 632–635
Krouskop TA, Wheeler TM, Kallel F, Garra BS, Hall T (1998) Elastic moduli of breast and prostate tissues under compression. Ultrason Imaging 20(4):260–274
Nelder JA, Mead R (1965) A simplex method for function minimization. Comput J 7:308–313
Pressure Profiles Systems, Inc. Tactile Sensor Imaging Solutions in Medical Devices. www.pressureprofile.com/index-medical.php. Accessed 10 Jan 2013
Marks L, Young S, Natarajan S (2013) MRI-ultrasound fusion for guidance of targeted prostate biopsy. Curr Opin Urol 23(1):43–50
Acknowledgments
This research is supported by the Natural Sciences and Engineering Research Council (NSERC) of Canada, Computer-Assisted Medical Interventions at Western University funded by NSERC Collaborative Research and Training Experience (CREATE) and internal funding by Western University, London, Ontario.
Conflict of Interest
There is no conflict of interest in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mousavi, S.R., Raahemifar, K., Pautler, S. et al. Towards ultrasound probe positioning optimization during prostate needle biopsy using pressure feedback. Int J CARS 8, 1053–1061 (2013). https://doi.org/10.1007/s11548-013-0898-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-013-0898-3