Abstract
Purpose
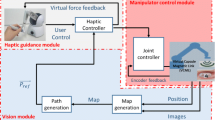
Tele-operation of robotic surgery reduces the radiation exposure during the interventional radiological operations. However, endoscope vision without force feedback on the surgical tool increases the difficulty for precise manipulation and the risk of tissue damage. The shared control of vision and force provides a novel approach of enhanced control with haptic guidance, which could lead to subtle dexterity and better maneuvrability during MIS surgery.
Methods
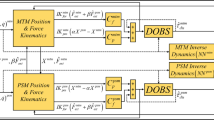
The paper provides an innovative shared control method for robotic minimally invasive surgery system, in which vision and haptic feedback are incorporated to provide guidance cues to the clinician during surgery. The incremental potential field (IPF) method is utilized to generate a guidance path based on the anatomy of tissue and surgical tool interaction. Haptic guidance is provided at the master end to assist the clinician during tele-operative surgical robotic task.
Results
The approach has been validated with path following and virtual tumor targeting experiments. The experiment results demonstrate that comparing with vision only guidance, the shared control with vision and haptics improved the accuracy and efficiency of surgical robotic manipulation, where the tool-position error distance and execution time are reduced.
Conclusions
The validation experiment demonstrates that the shared control approach could help the surgical robot system provide stable assistance and precise performance to execute the designated surgical task. The methodology could also be implemented with other surgical robot with different surgical tools and applications.












Similar content being viewed by others
References
Uçar BY (2012) Percutaneous surgery: A safe procedure for trigger finger? N Am J Med Sci 4(9):401
DiMaio SP, Salcudean SE (2005) Interactive simulation of needle insertion models. Biomed Eng IEEE Trans 52(7):1167–1179
Lanfranco AR, Castellanos AE, Desai JP, Meyers WC (2004) Robotic surgery: a current perspective. Ann surg 239(1):14–21. doi:10.1097/01.sla.0000103020.19595.7d
Xiong L, Chui C, Teo C, Lau D (2013) Incremental potential field based haptic guidance for medical simulation. In: IEEE/SICE international symposium on system integration (SII). IEEE, pp 772–777
Xiong L, Chui C-K, Fu Y, Teo C-L, Li Y (2015) Modeling of human artery tissue with probabilistic approach. Comput Biol Med 59:152–159
Marescaux J, Smith MK, Fölscher D, Jamali F, Malassagne B, Leroy J (2001) Telerobotic laparoscopic cholecystectomy: initial clinical experience with 25 patients. Ann Surg 234(1):1
Marescaux J, Leroy J, Rubino F, Smith M, Vix M, Simone M, Mutter D (2002) Transcontinental robot-assisted remote telesurgery: feasibility and potential applications. Ann Surg 235(4):487
Yamamoto T, Abolhassani N, Jung S, Okamura AM, Judkins TN (2012) Augmented reality and haptic interfaces for robot—assisted surgery. Int J Med Robot Comput Assist Surg 8(1):45–56
Okamura AM (2009) Haptic feedback in robot-assisted minimally invasive surgery. Curr Opin Urol 19(1):102–107
Lamata P, Freudenthal A, Cano A, Kalkofen D, Schmalstieg D, Naerum E, Samset E, Gómez EJ, Sánchez-Margallo FM, Furtado H (2010) Augmented reality for minimally invasive surgery: overview and some recent advances. INTECH Open Access Publisher, Vienna
Suzuki S, Suzuki N, Hattori A, Hayashibe M, Konishi K, Kakeji Y, Hashizume M (2005) Tele-surgery simulation with a patient organ model for robotic surgery training. Int J Med Robot Comput Assist Surg 1(4):80–88
Ming L, Ishii M, Taylor RH (2007) Spatial motion constraints using virtual fixtures generated by anatomy. Robot IEEE Trans 23(1):4–19
Wagner CR, Stylopoulos N, Howe RD (2002) The role of force feedback in surgery: analysis of blunt dissection. In: Symposium on haptic interfaces for virtual environment and teleoperator systems. Citeseer, pp 73–79
Kübler B, Seibold U, Hirzinger G (2005) Development of actuated and sensor integrated forceps for minimally invasive robotic surger. Int J Med Robot Comput Assist Surg 1(3):96–107
Ribeiro F, Lopes A (2013) Haptic guidance in a collaborative robotic system. In: Neto P, Moreira A (eds) Robotics in smart manufacturing, vol 371., Communications in computer and information scienceSpringer, Berlin, pp 101–112
Powell D, O’Malley MK (2012) The task-dependent efficacy of shared-control haptic guidance paradigms. Haptics IEEE Trans 5(3):208–219
Bowyer SA, Davies BL, Rodriguez y, Baena F (2014) Active constraints/virtual fixtures: a survey. Robot IEEE Trans 30(1):138–157
Li M, Ishii M, Taylor RH (2007) Spatial motion constraints using virtual fixtures generated by anatomy. Robot IEEE Trans 23(1):4–19
Safavi A, Zadeh MH (2015) Model-based haptic guidance in surgical skill improvement. In: Systems, man, and cybernetics (SMC), 2015 IEEE international conference on, 9-12 Oct. 2015, pp 1104–1109
Yang T, Liu J, Huang W, Yang L, Chui CK, Ang Jr MH, Su Y, Chang SK (2013) Mechanism of a learning robot manipulator for laparoscopic surgical training. In: Frontiers of intelligent autonomous systems. Springer, pp 297–308
Sawashima H, Hori Y, Sunahara H, Oie Y (1997) Characteristics of UDP packet loss: effect of tcp traffic. In: Proceedings of INET’97: the seventh annual conference of the internet society
Ge SS, Cui YJ (2002) Dynamic motion planning for mobile robots using potential field method. Auton Robots 13(3):207–222
Latombe JC (2012) Robot motion planning (Vol. 124). Springer Science & Business Media, Newyork
Koren Y, Borenstein J (1991) Potential field methods and their inherent limitations for mobile robot navigation. In: Robotics and automation, 1991. Proceedings 1991 IEEE international conference on, IEEE, pp 1398–1404
Xiong L, Chui C-K, Teo C-L (2013) Reality based modeling and simulation of gallbladder shape deformation using variational methods. Int J Comput Assist Radiol Surg 8(5):857–865
Cleary K, Nguyen C (2001) State of the art in surgical robotics: clinical applications and technology challenges. Comput Aid Surg 6(6):312–328
Rossi A, Trevisani A, Zanotto V (2005) A telerobotic haptic system for minimally invasive stereotactic neurosurgery. Int J Med Robot Comput Assist Surg 1(2):64–75
Kesner SB, Howe RD (2014) Robotic catheter cardiac ablation combining ultrasound guidance and force control. Int J Robot Res 33(4):631–644
Cole GA, Harrington K, Su H, Camilo A, Pilitsis JG, Fischer GS (2014) Closed-loop actuated surgical system utilizing real-time in-situ MRI guidance. In: Experimental Robotics. Springer, pp 785–798
Webster RJ, Memisevic J, Okamura AM (2005) Design considerations for robotic needle steering. In: Robotics and automation, 2005. ICRA 2005. Proceedings of the 2005 IEEE international conference on, 18–22 April 2005, pp 3588–3594
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Xiong, L., Chng, C.B., Chui, C.K. et al. Shared control of a medical robot with haptic guidance. Int J CARS 12, 137–147 (2017). https://doi.org/10.1007/s11548-016-1425-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-016-1425-0