Abstract
Purpose
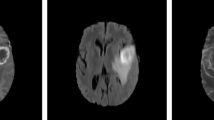
Intraoperative ultrasound (iUS) imaging is commonly used to support brain tumor operation. The tumor segmentation in the iUS images is a difficult task and still under improvement because of the low signal-to-noise ratio. The success of automatic methods is also limited due to the high noise sensibility. Therefore, an alternative brain tumor segmentation method in 3D-iUS data using a tumor model obtained from magnetic resonance (MR) data for local MR–iUS registration is presented in this paper. The aim is to enhance the visualization of the brain tumor contours in iUS.
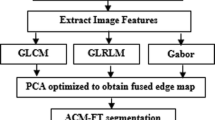
Methods
A multistep approach is proposed. First, a region of interest (ROI) based on the specific patient tumor model is defined. Second, hyperechogenic structures, mainly tumor tissues, are extracted from the ROI of both modalities by using automatic thresholding techniques. Third, the registration is performed over the extracted binary sub-volumes using a similarity measure based on gradient values, and rigid and affine transformations. Finally, the tumor model is aligned with the 3D-iUS data, and its contours are represented.
Results
Experiments were successfully conducted on a dataset of 33 patients. The method was evaluated by comparing the tumor segmentation with expert manual delineations using two binary metrics: contour mean distance and Dice index. The proposed segmentation method using local and binary registration was compared with two grayscale-based approaches. The outcomes showed that our approach reached better results in terms of computational time and accuracy than the comparative methods.
Conclusion
The proposed approach requires limited interaction and reduced computation time, making it relevant for intraoperative use. Experimental results and evaluations were performed offline. The developed tool could be useful for brain tumor resection supporting neurosurgeons to improve tumor border visualization in the iUS volumes.








Similar content being viewed by others
References
Noble JA, Boukerroui D (2006) Ultrasound image segmentation: a survey. IEEE Trans Med Imaging 25(8):987–1010
Xian M, Zhang Y, Cheng H (2015) Fully automatic segmentation of breast ultrasound images based on breast characteristics in space and frequency domains. Pattern Recognit 48(2):485–497
Huang Q, Bai X, Li Y, Jin L, Li X (2014) Optimized graph-based segmentation for ultrasound images. Neurocomputing 129:216–224
Huang Q-H, Lee S-Y, Liu L-Z, Lu M-H, Jin L-W, Li A-H (2012) A robust graph-based segmentation method for breast tumors in ultrasound images. Ultrasonics 52(2):266–275
Huang Q, Luo Y, Zhang Q (2017) Breast ultrasound image segmentation: a survey. Int J Comput Assist Radiol Surg 12(3):493–507
Qiu W, Chen Y, Kishimoto J, de Ribaupierre S, Chiu B, Fenster A, Yuan J (2017) Automatic segmentation approach to extracting neonatal cerebral ventricles from 3d ultrasound images. Med Image Anal 35:181–191
Yu Y, Chen Y, Chiu B (2016) Fully automatic prostate segmentation from transrectal ultrasound images based on radial bas-relief initialization and slice-based propagation. Comput Biol Med 74:74–90
Li X, Li C, Fedorov A, Kapur T, Yang X (2016) Segmentation of prostate from ultrasound images using level sets on active band and intensity variation across edges. Med Phys 43(6):3090–3103. https://doi.org/10.1118/1.4950721
Ghose S, Oliver A, Mitra J, Mart R, Llad X, Freixenet J, Sidib D, Vilanova JC, Comet J, Meriaudeau F (2013) A supervised learning framework of statistical shape and probability priors for automatic prostate segmentation in ultrasound images. Med Image Anal 17(6):587–600
Bersvendsen J, Orderud F, Massey RJ, Foss K, Gerard O, Urheim S, Samset E (2016) Automated segmentation of the right ventricle in 3d echocardiography: a kalman filter state estimation approach. IEEE Trans Med Imaging 35(1):42–51
Bernard O, Bosch JG, Heyde B, Alessandrini M, Barbosa D, Camarasu-Pop S, Cervenansky F, Valette S, Mirea O, Bernier M, Jodoin PM, Domingos JS, Stebbing RV, Keraudren K, Oktay O, Caballero J, Shi W, Rueckert D, Milletari F, Ahmadi SA, Smistad E, Lindseth F, van Stralen M, Wang C, Smedby O, Donal E, Monaghan M, Papachristidis A, Geleijnse ML, Galli E, D’hooge J (2016) Standardized evaluation system for left ventricular segmentation algorithms in 3d echocardiography. IEEE Trans Med Imaging 35(4):967–977
Huang J, Yang X, Chen Y, Tang L (2013) Ultrasound kidney segmentation with a global prior shape. J Vis Commun Image Represent 24(7):937–943
Destrempes F, Cardinal M-HR, Allard L, Tardif J-C, Cloutier G (2014) Segmentation method of intravascular ultrasound images of human coronary arteries. Comput Med Imaging Graph 38(2):91–103 Special Issue on Computing and Visualisation for Intravascular Imaging
Sun S, Sonka M, Beichel RR (2013) Graph-based ivus segmentation with efficient computer-aided refinement. IEEE Trans Med Imaging 32(8):1536–1549
Chalopin C, Krissian K, Meixensberger J, Müns A, Arlt F, Lindner D (2013) Evaluation of a semi-automatic segmentation algorithm in 3D intraoperative ultrasound brain angiography. Biomed Tech 58(3):293–302
Ilunga-Mbuyamba E, Avina-Cervantes JG, Lindner D, Cruz-Aceves I, Arlt F, Chalopin C (2016) Vascular structure tracking in intraoperative 3D contrast-enhanced ultrasound data. Sensors 16(4):1–14
Rueda S, Fathima S, Knight CL, Yaqub M, Papageorghiou AT, Rahmatullah B, Foi A, Maggioni M, Pepe A, Tohka J, Stebbing RV, McManigle JE, Ciurte A, Bresson X, Cuadra MB, Sun C, Ponomarev GV, Gelfand MS, Kazanov MD, Wang CW, Chen HC, Peng CW, Hung CM, Noble JA (2014) Evaluation and comparison of current fetal ultrasound image segmentation methods for biometric measurements: a grand challenge. IEEE Trans Med Imaging 33(4):797–813
Dahdouh S, Angelini ED, Grang G, Bloch I (2015) Segmentation of embryonic and fetal 3d ultrasound images based on pixel intensity distributions and shape priors. Med Image Anal 24(1):255–268
Berton F, Cheriet F, Miron M-C, Laporte C (2016) Segmentation of the spinous process and its acoustic shadow in vertebral ultrasound images. Comput Biol Med 72:201–211
Aventaggiato M, Conversano F, Pisani P, Casciaro E, Franchini R, Lay-Ekuakille A, Muratore M, Casciaro S (2016) Validation of an automatic segmentation method to detect vertebral interfaces in ultrasound images. IET Sci Meas Technol 10(1):18–27
Ma J, Wu F, Jiang T, Zhao Q, Kong D (2017) Ultrasound image-based thyroid nodule automatic segmentation using convolutional neural networks. Int J Comput Assist Radiol Surg 12(11):1895–1910. https://doi.org/10.1007/s11548-017-1649-7
Lian J, Ma Y, Ma Y, Shi B, Liu J, Yang Z, Guo Y (2017) Automatic gallbladder and gallstone regions segmentation in ultrasound image. Int J Comput Assist Radiol Surg 12(4):553–568. https://doi.org/10.1007/s11548-016-1515-z
Ritschel K, Pechlivanis I, Winter S (2015) Brain tumor classification on intraoperative contrast-enhanced ultrasound. Int J Comput Assist Radiol Surg 10(5):531–540. https://doi.org/10.1007/s11548-014-1089-6
Reinertsen I, Lindseth F, Unsgaard G, Collins D (2007) Clinical validation of vessel-based registration for correction of brain-shift. Med Image Anal 11(6):673–684 [Online]. Available: http://www.sciencedirect.com/science/article/pii/S1361841507000679
Muns A, Meixensberger J, Arnold S, Schmitgen A, Arlt F, Chalopin C, Lindner D (2011) Integration of a 3d ultrasound probe into neuronavigation. Acta Neurochir 153(7):1529–1533. https://doi.org/10.1007/s00701-011-0994-5
Unsgaard G, Selbekk T, Brostrup Muller T, Ommedal S, Torp SH, Myhr G, Bang J, Nagelhus Hernes TA (2005) Ability of navigated 3d ultrasound to delineate gliomas and metastases—comparison of image interpretations with histopathology. Acta Neurochir 147(12):1259–1269. https://doi.org/10.1007/s00701-005-0624-1
Farhat N, Kapur T, Kikinis R (2015) Chapter 6—role of computers and image processing in image-guided brain tumor surgery. In: Golby AJ (ed) Image-guided neurosurgery. Academic Press, Boston, pp 143–161
Chang H, Chen Z, Huang Q, Shi J, Li X (2015) Graph-based learning for segmentation of 3d ultrasound images. Neurocomputing 151:632–644 Part 2
Hodneland E, Lundervold A, Rrvik J, Munthe-Kaas AZ (2014) Normalized gradient fields for nonlinear motion correction of dce-mri time series. Comput Med Imaging Graph 38(3):202–210
Fischer B, Modersitzki J (2008) Ill-posed medicinean introduction to image registration. Inverse Probl 24(3):034008
Fuerst B, Wein W, Mueller M, Navab N (2014) Automatic ultrasound MRI registration for neurosurgery using the 2d and 3d LC2 metric. Med Image Anal 18(8):1312–1319. Special issue on the 2013 conference on medical image computing and computer assisted intervention
Rivaz H, Karimaghaloo Z, Fonov VS, Collins DL (2014) Nonrigid registration of ultrasound and mri using contextual conditioned mutual information. IEEE Trans Med Imaging 33(3):708–725
Hodneland E, Lundervold A, Rrvik J, Munthe-Kaas AZ, (2013) Normalized gradient fields and mutual information for motion correction of dce-mri images. In: 8th international symposium on image and signal processing and analysis (ISPA) Sept 2013, pp 516–521
Lai Z, Hu J, Liu C, Taimouri V, Pai D, Zhu J, Xu J, Hua J (2010) Intra-patient supine-prone colon registration in CT colonography using shape spectrum. In: Jiang T, Navab N, Pluim JPW, Viergever MA (eds) Medical image computing and computer-assisted intervention—MICCAI 2010: 13th international conference, Beijing, China, September 20–24, 2010, proceedings, part I, Springer Berlin Heidelberg, Berlin, Heidelberg, pp 332–339
Commandeur F, Simon A, Mathieu R, Nassef M, Ospina JD, Rolland Y, Haigron P, Crevoisier RD, Acosta O (2016) MRI to CT prostate registration for improved targeting in cancer external beam radiotherapy. IEEE J Biomed Health Inform 1(99):1
Liu JF, Cui FS, Liu ZJ, Liu JM (2015) A technique for prostate registration by finite element modeling. In: Jaffray DA (ed) World congress on medical physics and biomedical engineering, June 7–12, 2015, Toronto, Canada. Springer International Publishing, Cham, pp 870–873
Xu R, Athavale P, Nachman A, Wright GA (2014) Multiscale registration of real-time and prior mri data for image-guided cardiac interventions. IEEE Trans Biomed Eng 61(10):2621–2632
Ng H-F (2006) Automatic thresholding for defect detection. Pattern Recognit Lett 27(14):1644–1649
Otsu N (1979) A threshold selection method from gray-level histograms. IEEE Trans Syst Man Cybern 9(1):62–66
Riva M, Hennersperger C, Milletari F, Katouzian A, Pessina F, Gutierrez-Becker B, Castellano A, Navab N, Bello L (2017) 3D intra-operative ultrasound and MR image guidance: pursuing an ultrasound-based management of brainshift to enhance neuronavigation. Int J Comput Assist Radiol Surg 12(10):1711–1725
Haber E, Modersitzki J (2006) Intensity gradient based registration and fusion of multi-modal images. In: Larsen R, Nielsen M, and Sporring J (eds) Medical image computing and computer-assisted intervention—MICCAI 2006: 9th international conference, Copenhagen, Denmark, October 1–6, 2006. Proceedings, Part II, Springer, Berlin, Heidelberg pp 726–733
Modersitzki J (2009) Fair: flexible algorithms for image registration. Society for Industrial and Applied Mathematics, Philadelphia
Meng Q, Lu X, Zhang B, Gu Y, Ren G, Huang X (2018) Research on the ROI registration algorithm of the cardiac CT image time series. Biomed Signal Process Control 40:71–82
Farnia P, Ahmadian A, Shabanian T, Serej ND, Alirezaie J (2015) Brain-shift compensation by non-rigid registration of intra-operative ultrasound images with preoperative MR images based on residual complexity. Int J Comput Assist Radiol Surg 10(5):555–562
Acknowledgements
Authors thank the University of Guanajuato for the provided financial support that allows concluding this research. Additionally, we would like to thank the department of neurosurgery, University Hospital Leipzig, for the clinical study and data collection in the context of an earlier research project funded by the German Research Society (Deutsche Forschungsgemeinschaft).
Funding
This work has been funded by the Mexican Council on Science and Technology (CONACyT) (Grant Number 493442).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. For this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Ilunga-Mbuyamba, E., Avina-Cervantes, J.G., Lindner, D. et al. Patient-specific model-based segmentation of brain tumors in 3D intraoperative ultrasound images. Int J CARS 13, 331–342 (2018). https://doi.org/10.1007/s11548-018-1703-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-018-1703-0