Abstract
Purpose
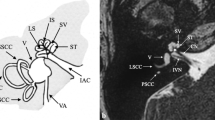
Surgical removal of pathology at the lateral skull base is challenging because of the proximity of critical anatomical structures which can lead to significant morbidity when damaged or traversed. Pre-operative computed surgical approach planning has the potential to aid in selection of the optimal approach to remove pathology and minimize complications.
Methods
We propose an automated surgical approach planning algorithm to derive the optimal approach to vestibular schwannomas in the internal auditory canal for hearing preservation surgery. The algorithm selects between the middle cranial fossa and retrosigmoid approach by utilizing a unique segmentation of each patient’s anatomy and a cost function to minimize potential surgical morbidity.
Results
Patients who underwent hearing preservation surgery for vestibular schwannoma resection (n = 9) were included in the cohort. Middle cranial fossa surgery was performed in 5 patients, and retrosigmoid surgery was performed in 4. The algorithm favored the performed surgical approach in 6 of 9 patients.
Conclusion
We developed a method for computing morbidity costs of surgical paths to objectively analyze surgical approaches at the lateral skull base. Computed pre-operative planning may assist in surgical decision making, trainee education, and improving clinical outcomes.





Similar content being viewed by others
Availability of data and material
Data used for this study are currently not publicly available.
Code availability
Code is available per request to authors.
References
Aghdasi N, Whipple M, Humphreys IM, Moe KS, Hannaford B, Bly RA (2018) Automated surgical approach planning for complex skull base targets: development and validation of a cost function and semantic At-las. Surg Innov 25(5):476–484. https://doi.org/10.1177/1553350618782287
Banalagay RA, Labadie RF, Chakravorti S, Noble JH (2020) Insertion depth for optimized positioning of precurved cochlear implant electrodes. Otol Neurotol 41(8):1066–1071. https://doi.org/10.1097/MAO.0000000000002726
Bly RA, Su D, Hannaford B, Ferreira M Jr, Moe KS (2012) Computer modeled multiportal approaches to the skull base. J Neurol Surg B Skull Base. 73(6):415–423. https://doi.org/10.1055/s-0032-1329623
Cousins V (2008) Lateral skull base surgery: a complicated pursuit? J Laryngol Otol 122(3):221–229. https://doi.org/10.1017/S0022215107000436
Davey M, McInerney NM, Barry T, Hussey A, Potter S (2019) Virtual surgical planning computer-aided design-guided osteocutaneous fibular free flap for craniofacial reconstruction: a novel surgical approach. Cureus 11(11):e6256. https://doi.org/10.7759/cureus.6256
Driscoll CL, Jackler RK, Pitts LH, Banthia V (2000) Is the entire fundus of the internal auditory canal visible during the middle fossa approach for acoustic neuroma? Otol Neurotol 21(3):382–388
Dos Santos LR, Cernea CR, Brandao LG, Siqueira MG, Vellutini EA, Velazco OP, Cruz OL, Morais-Besteiro J, Freitas CA (1994) Results and prognostic factors in skull base surgery. Am J Surg 168(5):481–484. https://doi.org/10.1016/s0002-9610(05)80106-0
Fayad JN, Friedman RA, Schwartz MS (2012) The retrosigmoid approach In: Lateral Skull Base Surgery: House Clinic Atlas. NY: Theime: New York
Fauser J, Stenin I, Bauer M, Hsu WH, Kristin J, Klenzner T, Schipper J, Mukhopadhyay A (2019) Toward an automatic preoperative pipeline for image-guided temporal bone surgery. Int J Comput Assist Radiol Surg 14(6):967–976. https://doi.org/10.1007/s11548-019-01937-x
Fedorov A, Beichel R, Kalpathy-Cramer J, Finet J, Fillion-Robin J-C, Pujol S, Bauer C, Jennings D, Fennessy F, Sonka M, Buatti J, Aylward SR, Miller JV, Pieper S, Kikinis R (2012) 3D Slicer as an image computing platform for the quantitative imaging network. Magn Reson Imaging 30(9):1323–1341 (PMID: 22770690)
Friedman RA, Fayad JN (2012) The middle cranial fossa approach to vestibular schwannomas. In: Lateral Skull Base Surgery: House Clinic Atlas. New York, NY; Theime
Gerber N, Bell B, Gavaghan K, Weisstanner C, Caversaccio M, Weber S (2014) Surgical planning tool for robotically assisted hearing aid implantation. Int J Comput Assist Radiol Surg 9(1):11–20. https://doi.org/10.1007/s11548-013-0908-5
Halliday J, Rutherford SA, McCabe MG, Evans DG (2018) An update on the diagnosis and treatment of vestibular schwannoma. Expert Rev Neurother 18(1):29–39. https://doi.org/10.1080/14737175.2018.1399795 (Epub 2017 Nov 7)
Helck A, Schumann C, Aumann J, Thierfelder K, Strobl FF, Braunagel M, Niethammer M, Clevert DA, Hoffmann RT, Reiser M, Sandner T, Trumm C (2016) Automatic path proposal computation for CT-guided percutaneous liver biopsy. Int J Comput Assist Radiol Surg 11(12):2199–2205. https://doi.org/10.1007/s11548-015-1349-0
Kaul V, Cosetti MK (2018) Management of vestibular schwannoma (Including NF2): facial nerve considerations. Otolaryngol Clin North Am 51(6):1193–1212. https://doi.org/10.1016/j.otc.2018.07.015
Kohlberg GD, Lipschitz N, Raghavan AM, Breen JT, Pensak ML, Zuccarello M, Samy RN (2021) Middle cranial fossa approach to vestibular schwannoma resection in the older patient population. Otol Neurotol. https://doi.org/10.1097/MAO.0000000000002881
Konuthula N, Parikh SR, Bly RA (2020) Robotics in pediatric otolaryngology-head and neck surgery and advanced surgical planning. Otolaryngol Clin North Am 53(6):1005–1016. https://doi.org/10.1016/j.otc.2020.07.011
LaRouere MJ, Seilesh BC, Bojrab DI (2015) Surgical techniques in otolaryngology -Head and neck surgery:otologic and neurootologic surgery, Jaypee Brothers Medical Publishers. ProQuest Ebook Central
Lipschitz N, Kohlberg GD, Tawfik KO, Walters ZA, Breen JT, Zuccarello M, Andaluz N, Dinapoli VA, Pensak ML, Samy RN (2019) Cerebrospinal fluid leak rate after vestibular schwannoma surgery via middle cranial fossa approach. J Neurol Surg B Skull Base 80(4):437–440. https://doi.org/10.1055/s-0038-1675752
Lipschitz N, Kohlberg GD, Walters ZA, Tawfik KO, Samy RN, Pensak ML, Zuccarello M, Andaluz N, Dinapoli VA, Breen JT (2019) Obesity is not associated with postoperative complications after vestibular schwannoma surgery in a large single institution series. Otol Neurotol 40(10):1373–1377. https://doi.org/10.1097/MAO.0000000000002397
Neves CA, Tran ED, Kessler IM, Blevins NH (2021) Fully automated preoperative segmentation of temporal bone structures from clinical CT scans. Sci Rep 11:116. https://doi.org/10.1038/s41598-020-80619-0
Meyer TA, Canty PA, Wilkinson EP, Hansen MR, Rubinstein JT, Gantz BJ (2006) Small acoustic neuromas: surgical outcomes versus observation or radiation. Otol Neurotol 27(3):380–392
Raghavan AM, Lipschitz N, Kohlberg GD, Samy RN, Zuccarello M, Pensak ML, Breen JT (2020) Is longer surgery more dangerous? operative duration not associated with complications after vestibular schwannoma resection. Otol Neurotol 41(2):e268–e272. https://doi.org/10.1097/MAO.0000000000002510
Rathgeb C, Anschuetz L, Schneider D, Dür C, Caversaccio M, Weber S, Williamson T (2018) Accuracy and feasibility of a dedicated image guidance solution for endoscopic lateral skull base surgery. Eur Arch Otorhinolaryngol 275(4):905–911. https://doi.org/10.1007/s00405-018-4906-7
Saliba J, Friedman RA, Cueva RA (2019) Hearing preservation in vestibular schwannoma surgery. J Neurol Surg B Skull Base 80(2):149–155. https://doi.org/10.1055/s-0038-1677550
Schick B, Dlugaiczyk J (2013) Surgery of the ear and the lateral skull base: pitfalls and complications. GMS Curr Top Otorhinolaryngol Head Neck Surg. https://doi.org/10.3205/cto000097
Shapey J, Kujawa A, Dorent R, Wang G, Dimitriadis A, Grishchuk D, Paddick I, Kitchen N, Bradford R, Saeed SR, Bisdas S, Ourselin S, Vercauteren T (2021) Segmentation of vestibular schwannoma from MRI, an open annotated dataset and baseline algorithm. Sci Data 8(1):286. https://doi.org/10.1038/s41597-021-01064-w
Shapey J, Wang G, Dorent R, Dimitriadis A, Li W, Paddick I, Kitchen N, Bisdas S, Saeed SR, Ourselin S, Bradford R, Vercauteren T (2019) An artificial intelligence framework for automatic segmentation and volumetry of vestibular schwannomas from contrast-enhanced T1-weighted and high-resolution T2-weighted MRI. J Neurosurg. https://doi.org/10.3171/2019.9.JNS191949
Wilkinson EP, Roberts DS, Cassis A, Schwartz MS (2016) Hearing outcomes after middle fossa or retrosigmoid craniotomy for vestibular schwannoma tumors. J Neurol Surg B Skull Base 77(04):333–340
Zanoletti E, Martini A, Emanuelli E, Mazzoni A (2012) Lateral approaches to the skull base. Acta Otorhinolaryngol Ital 32(5):281
Acknowledgements
Jason R. Crossley assisted in manuscript preparation.
Funding
Partial financial support was received from the Center for Translational Research–Clinical Research Scholars Program at Seattle Children’s Hospital.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors have no conflicts of interest to declare that are relevant to the content of this article.
Ethical approval
Approval for the study was obtained by the University of Washington Institutional Review Board.
Informed consent
All patient imaging was de-identified.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Rajesh, A.E., Rubinstein, J.T., Ferreira, M. et al. Automated objective surgical planning for lateral skull base tumors. Int J CARS 17, 427–436 (2022). https://doi.org/10.1007/s11548-022-02564-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11548-022-02564-9