Abstract
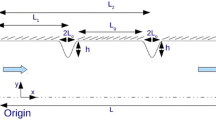
Considering the shear-thinning feature of blood viscosity, the characteristics of non-Newtonian fluids are important in pulsatile blood flows. Stenosis, with an abnormal narrowing of the vessel, blocks blood flow to downstream tissues and leads to plaque rupture. In smaller arteries of diameters up to a few hundred micrometers, such stenosis can result in severe consequences. Therefore, a systematic analysis of the blood flow around the stenosed microchannel is important. In this study, non-Newtonian behaviors of the blood flow around a microchannel of diameter 500 μm, with 60% severe stenosis, were examined using CFX under pulsatile flow condition, with a period of 1 s and Reynolds number of 14.025 at the systolic phase. The viscosity information of the two non-Newtonian samples and the used pulsatile profile were based on our previous study. For comparison, water at room temperature was used as the Newtonian fluid. During the pulsatile phase, wall shear stress (WSS) is highly oscillated. In the case of the water flow, the recirculation occurred downstream the stenosis. This recirculation made the vortex structures travel the longest and induced a low WSS distribution and rapid normalized pressure drop at downstream of the stenosis. Conversely, the non-Newtonian feature of viscosity made flow structures almost symmetric, with respect to the stenosis. However, the highly oscillating WSS enhances the tendency of plaque instability and damage to the endothelium. Our findings on the influence of blood viscosity on stenotic lesions may help clinicians understand relevant mechanisms.
Graphic abstract









Similar content being viewed by others
References
Ahmed B (2014) New insights into the pathophysiology, classification, and diagnosis of coronary microvascular dysfunction. Coron Artery Dis 25:439–449
Amornsamankul S, Wiwatanapataphee B, Wu YH, Lenbury Y (2006) Effect of non-Newtonian behaviour of blood on pulsatile flows in stenotic arteries. Int J Biomed Sci 1:42–46
Anastasiou AD, Spyrogianni AS, Koskinas KC, Giannoglou GD, Paras SV (2012) Experimental investigation of the flow of a blood analogue fluid in a replica of a bifurcated small artery. Med Eng Phys 34:211–218
Arduini D, Rizzo G (1990) Normal values of pulsatility index front fetal vessels: a cross-sectional study on 1556 healthy fetuses. J Perinat Med Off J WAPM 18:165–172
Bishop JJ, Nance PR, Popel AS, Intaglietta M, Johnson PC (2001a) Effect of erythrocyte aggregation on velocity profiles in venules. Am J Physiol Heart Circ Physiol 280:H222–H236
Bishop JJ, Popel AS, Intaglietta M, Johnson PC (2001b) Rheological effects of red blood cell aggregation in the venous network: a review of recent studies. Biorheology 38:263–274
Bryan MT, Duckles H, Feng S, Hsiao ST, Kim HR, Serbanovic-Canic J, Evans PC (2014) Mechanoresponsive networks controlling vascular inflammation. Arterioscler Thromb Vasc Biol 34:2199–2205
Cheng C, Tempel D, Van Haperen R, Van Der Baan A, Grosveld F, Daemen MJ, Krams R, De Crom R (2006) Atherosclerotic lesion size and vulnerability are determined by patterns of fluid shear stress. Circulation 113:2744–2753
Chien S (1970) Shear dependence of effective cell volume as a determinant of blood viscosity. Science 168:977–979
Cowan AQ, Cho DJ, Rosenson RS (2012) Importance of blood rheology in the pathophysiology of atherothrombosis. Cardiovasc Drugs Ther 26:339–348
Dolan JM, Kolega J, Meng H (2013) High wall shear stress and spatial gradients in vascular pathology: a review. Ann Biomed Eng 41:1411–1427
Downing GJ, Yarlagadda AP, Maulik D (1991) Comparison of the pulsatility index and input impedance parameters in a model of altered hemodynamics. J Ultrasound Med 10:317–321
Gijsen FJ, Wentzel JJ, Thury A, Mastik F, Schaar JA, Schuurbiers JC, Slager CJ, Van Der Giessen WJ, De Feyter PJ, Van Der Steen AF, Serruys PW (2008) Strain distribution over plaques in human coronary arteries relates to shear stress. Am J Physiol Heart Circ Physiol 295:H1608–H1614
Glagov S, Weisenberg E, Zarins CK, Stankunavicius R, Kolettis GJ (1987) Compensatory enlargement of human atherosclerotic coronary arteries. N Engl J Med 316:1371–1375
Hong H, Song JM, Yeom E (2019) Variations in pulsatile flow around stenosed microchannel depending on viscosity. PLoS one 14:e0210993
Hunt JC, Wray AA, Moin P (1988) Eddies, streams, and convergence zones in turbulent flows. Center for Turbulence Research Report, CTR-S88, 193
Jahangiri M, Haghani A, Ghaderi R, Harat SMH (2018) Effect of non-Newtonian models on blood flow in artery with different consecutive stenosis. Int J Adv Des Manuf Technol 11:89–96
Jung SY, Yeom E (2017) Microfluidic measurement for blood flow and platelet adhesion around a stenotic channel: effects of tile size on the detection of platelet adhesion in a correlation map. Biomicrofluidics 11:024119
Justo D, Mashav N, Arbel Y, Kinori M, Steinvil A, Swartzon M, Molat B, Halkin A, Finkelstein A, Heruti R, Banai S (2009) Increased erythrocyte aggregation in men with coronary artery disease and erectile dysfunction. Int J Impot Res 21:192–197
Kang D, Song JM, Yeom E (2019) Design of microfluidic viscometer based on pressure estimation. J Vis 22:25–34
Kwak BR, Back M, Bochaton-Piallat ML, Caligiuri G, Daemen MJ, Davies PF, Hoefer IE, Holvoet P, Jo H, Krams R, Lehoux S, Monaco C, Steffens S, Virmani R, Weber C, Wentzel JJ, Evans PC (2014) Biomechanical factors in atherosclerosis: mechanisms and clinical implications. Eur Heart J 35:3013–3020
Lanza GA, Crea F (2010) Primary coronary microvascular dysfunction: clinical presentation, pathophysiology, and management. Circulation 121:2317–2325
Lima R, Wada S, Tanaka S, Takeda M, Ishikawa T, Tsubota KI, Imai Y, Yamaguchi T (2008) In vitro blood flow in a rectangular pdms microchannel: experimental observations using a confocal micro-PIV system. Biomed Microdevices 10:153–167
Lutz RJ, Cannon JN, Bischoff KB, Dedrick RL, Stiles RK, Fry DL (1977) Wall shear stress distribution in a model canine artery during steady flow. Circ Res 41:391–399
Malek AM, Alper SL, Izumo S (1999) Hemodynamic shear stress and its role in atherosclerosis. JAMA 282:2035–2042
Molla MM, Paul MC (2012) Les of non-Newtonian physiological blood flow in a model of arterial stenosis. Med Eng Phys 34:1079–1087
Nejad AA, Talebi Z, Cheraghali D, Shahbani-Zahiri A, Norouzi M (2018) Pulsatile flow of non-Newtonian blood fluid inside stenosed arteries: investigating the effects of viscoelastic and elastic walls, arteriosclerosis, and polycythemia diseases. Comput Methods Programs Biomed 154:109–122
Ong PK, Namgung B, Johnson PC, Kim S (2010) Effect of erythrocyte aggregation and flow rate on cell-free layer formation in arterioles. Am J Physiol Heart Circ Physiol 298:H1870–H1878
Rabby MG, Razzak A, Molla MM (2013) Pulsatile non-Newtonian blood flow through a model of arterial stenosis. Procedia Eng 56:225–231
Rainer C, Kawanishi DT, Chandraratna PA, Bauersachs RM, Reid CL, Rahimtoola SH, Meiselman HJ (1987) Changes in blood rheology in patients with stable angina pectoris as a result of coronary artery disease. Circulation 76:15–20
Schoenhagen P, Ziada KM, Kapadia SR, Crowe TD, Nissen SE, Tuzcu EM (2000) Extent and direction of arterial remodeling in stable versus unstable coronary syndromes: an intravascular ultrasound study. Circulation 101:598–603
Steinman DA (2000) Simulated pathline visualization of computed periodic blood flow patterns. J Biomech 33:623–628
Tronc F, Mallat Z, Lehoux S, Wassef M, Esposito B, Tedgui A (2000) Role of matrix metalloproteinases in blood flow-induced arterial enlargement—interaction with NO. Arterioscler Thromb Vasc Biol 20:E120–E126
Tzima E, Irani-Tehrani M, Kiosses WB, Dejana E, Schultz DA, Engelhardt B, Cao GY, Delisser H, Schwartz MA (2005) A mechanosensory complex that mediates the endothelial cell response to fluid shear stress. Nature 437:426–431
Vahidkhah K, Balogh P, Bagchi P (2016) Flow of red blood cells in stenosed microvessels. Sci Rep 6:28194
Varnava AM, Mills PG, Davies MJ (2002) Relationship between coronary artery remodeling and plaque vulnerability. Circulation 105:939–943
Yeom E (2018) Different adhesion behaviors of platelets depending on shear stress around stenotic channels. J Vis 21:95–104
Yeom E, Lee SJ (2015) Relationship between velocity profile and ultrasound echogenicity in pulsatile blood flows. Clin Hemorheol Microcirc 59:197–209
Yeom E, Kang YJ, Lee SJ (2014) Changes in velocity profile according to blood viscosity in a microchannel. Biomicrofluidics 8:034110
Acknowledgements
This work was supported by Biomedical Research Institute Grant (2015-21), Pusan National University Hospital.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ha, Y.K., Hong, H., Yeom, E. et al. Numerical study of the pulsatile flow depending on non-Newtonian viscosity in a stenosed microchannel. J Vis 23, 61–70 (2020). https://doi.org/10.1007/s12650-019-00601-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12650-019-00601-5