Abstract
Background
Regarding the assessment of patients’ immune and nutritional status, prognostic nutritional index (PNI) has been reported as a predictive marker for surgical outcomes in various types of cancer. The aim of our study was to evaluate the effect of PNI in prognosis of gastric cancer patients submitted to curative-intent resectional surgery.
Material and methods
A retrospective analysis with 637 gastric cancer cases submitted to curative-intent surgery, between 2010 and 2017, in an upper GI surgery unit. We analyzed 396 patients that met the inclusion criteria for this study. The median follow-up was 37 (0–113) months.
Results
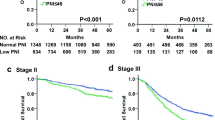
According to Youden’s method, the optimal PNI cutoff for OS was 41.625 (sensitivity 89.3% and specificity 41.3%). OS was significantly shorter in the lower-PNI group of patients when compared to the higher-PNI group (40.26 vs 77.49 months; p < 0.001). Higher PNI had a positive impact on OS in univariable analysis. When adjusted to pStage, higher PNI was still significantly associated with better OS (HR 0.405; CI 95% 0.253–0.649; p < 0.001). Regarding DFS, higher PNI was associated with better DFS (HR 0.421; CI 95% 0.218–0.815; p = 0.010). Higher-PNI group had a protective effect regarding postoperative morbidity and mortality.
Conclusions
In this cohort, PNI was disclosed to significantly impact GC patients’ OS and DFS, including in multivariable analysis when adjusting for classical prognostic features. PNI can be used to predict patients at increased risk of postoperative morbidity and mortality. This index may be of use in identifying candidate patients who would benefit from perioperative nutritional support to improve surgical outcomes.



Similar content being viewed by others
References
Bray F et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 68(6):394–424
Surveillance E, and End Results (SEER) Program (www.seer.cancer.gov) Research Data (1975-2016), National Cancer Institute, DCCPS, Surveillance Research Program, released April 2019, based on the November 2018 submission.
Kim HH et al (2010) Morbidity and mortality of laparoscopic gastrectomy versus open gastrectomy for gastric cancer: an interim report—a phase III multicenter, prospective, randomized trial (KLASS Trial). Ann Surg 251(3):417–420
Lee JY et al (2016) Clinical significance of the prognostic nutritional index for predicting short- and long-term surgical outcomes after gastrectomy: a retrospective analysis of 7781 gastric cancer patients. Medicine (Baltimore) 95(18):e3539
Park DJ et al (2005) Predictors of operative morbidity and mortality in gastric cancer surgery. Br J Surg 92(9):1099–1102
Inokuchi M et al (2014) Impact of comorbidities on postoperative complications in patients undergoing laparoscopy-assisted gastrectomy for gastric cancer. BMC Surg 14:97
Weimann A et al (2017) ESPEN guideline: clinical nutrition in surgery. Clin Nutr 36(3):623–650
Schiesser M et al (2009) The correlation of nutrition risk index, nutrition risk score, and bioimpedance analysis with postoperative complications in patients undergoing gastrointestinal surgery. Surgery 145(5):519–526
Guo W et al (2010) Screening of the nutritional risk of patients with gastric carcinoma before operation by NRS 2002 and its relationship with postoperative results. J Gastroenterol Hepatol 25(4):800–803
Buzby GP et al (1980) Prognostic nutritional index in gastrointestinal surgery. Am J Surg 139(1):160–167
Nozoe T et al (2002) Correlation of pre-operative nutritional condition with post-operative complications in surgical treatment for oesophageal carcinoma. Eur J Surg Oncol 28(4):396–400
Mohri Y et al (2013) Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg 37(11):2688–2692
Pinato DJ, North BV, Sharma R (2012) A novel, externally validated inflammation-based prognostic algorithm in hepatocellular carcinoma: the prognostic nutritional index (PNI). Br J Cancer 106(8):1439–1445
Migita K et al (2013) The prognostic nutritional index predicts long-term outcomes of gastric cancer patients independent of tumor stage. Ann Surg Oncol 20(8):2647–2654
Li J et al (2019) Prognostic nutritional index predicts outcomes of patients after gastrectomy for cancer: a systematic review and meta-analysis of nonrandomized studies. Nutr Cancer 71(4):557–568
Zhang Z et al. (2017) Evaluation of blood biomarkers associated with risk of malnutrition in older adults: a systematic review and meta-analysis. Nutrients. 9(8)
Balkwill F (2009) Tumour necrosis factor and cancer. Nat Rev Cancer 9(5):361–371
Ray-Coquard I et al (2009) Lymphopenia as a prognostic factor for overall survival in advanced carcinomas, sarcomas, and lymphomas. Cancer Res 69(13):5383–5391
Sakurai K et al (2016) Low preoperative prognostic nutritional index predicts poor survival post-gastrectomy in elderly patients with gastric cancer. Ann Surg Oncol 23(11):3669–3676
Deftereos I et al. (2021) Preoperative nutrition intervention in patients undergoing resection for upper gastrointestinal cancer: results from the multi-centre NOURISH point prevalence study. Nutrients 13(9)
Deftereos I et al (2020) Nutritional outcomes of patients undergoing resection for upper gastrointestinal cancer in Australian hospitals (NOURISH): protocol for a multicentre point prevalence study. BMJ Open 10(5):e035824
Deftereos I et al. (2021) Assessment of nutritional status and nutrition impact symptoms in patients undergoing resection for upper gastrointestinal cancer: results from the multi-centre NOURISH point prevalence study. Nutrients 13(10)
Deftereos I et al (2022) Adherence to ESPEN guidelines and associations with postoperative outcomes in upper gastrointestinal cancer resection: results from the multi-centre NOURISH point prevalence study. Clin Nutr ESPEN 47:391–398
Deftereos I et al. (2022) Health service nutrition practices and associations with clinical outcomes in patients undergoing resection for upper gastrointestinal cancer: results from the multi-centre NOURISH point prevalence study. J Hum Nutr Diet. https://doi.org/10.1111/jhn.13006. Online ahead of print
Yu J et al (2019) Effect of laparoscopic vs open distal gastrectomy on 3-year disease-free survival in patients with locally advanced gastric cancer: the CLASS-01 randomized clinical trial. JAMA 321(20):1983–1992
Kim HH et al (2019) Effect of laparoscopic distal gastrectomy vs open distal gastrectomy on long-term survival among patients with stage I gastric cancer: the KLASS-01 randomized clinical trial. JAMA Oncol 5(4):506–513
van der Veen A et al (2021) Laparoscopic versus open gastrectomy for gastric cancer (LOGICA): a multicenter randomized clinical trial. J Clin Oncol 39(9):978–989
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Jorge Nogueiro and Hugo Santos-Sousa are equal contributors.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Nogueiro, J., Santos-Sousa, H., Pereira, A. et al. The impact of the prognostic nutritional index (PNI) in gastric cancer. Langenbecks Arch Surg 407, 2703–2714 (2022). https://doi.org/10.1007/s00423-022-02627-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00423-022-02627-0