Abstract
Background There is wide recognition that, with the rapid implementation of electronic health records (EHRs), large data sets are available for research. However, essential standardized nursing data are seldom integrated into EHRs and clinical data repositories. There are many diverse activities that exist to implement standardized nursing languages in EHRs; however, these activities are not coordinated, resulting in duplicate efforts rather than building a shared learning environment and resources.
Objective The purpose of this paper is to describe the historical context of nursing terminologies, challenges to the use of nursing data for purposes other than documentation of care, and a national action plan for implementing and using sharable and comparable nursing data for quality reporting and translational research.
Methods In 2013 and 2014, the University of Minnesota School of Nursing hosted a diverse group of nurses to participate in the Nursing Knowledge: Big Data and Science to Transform Health Care consensus conferences. This consensus conference was held to develop a national action plan and harmonize existing and new efforts of multiple individuals and organizations to expedite integration of standardized nursing data within EHRs and ensure their availability in clinical data repositories for secondary use. This harmonization will address the implementation of standardized nursing terminologies and subsequent access to and use of clinical nursing data.
Conclusion Foundational to integrating nursing data into clinical data repositories for big data and science, is the implementation of standardized nursing terminologies, common data models, and information structures within EHRs. The 2014 National Action Plan for Sharable and Comparable Nursing Data for Transforming Health and Healthcare builds on and leverages existing, but separate long standing efforts of many individuals and organizations. The plan is action focused, with accountability for coordinating and tracking progress designated.
Keywords: nursing informatics, terminology, electro health records, consensus development conference, national health policy
INTRODUCTION
The core problems of healthcare access, quality, safety, efficiency, and effectiveness have been described by several landmark reports.1–6 These problems have been exacerbated by the recent financial crisis and by the urgent need to accommodate an estimated 32 million newly insured patients. In addition, the annual cost of harmful medical errors is estimated to be $17.1 billion (in 2008 dollars),7 and the 63.1% of preventable injuries caused by medical errors further exacerbates healthcare expenditures.8 New strategies and models to address these issues, challenges, and opportunities in the practice and delivery of healthcare are essential and have been outlined in multiple reports, including Building a Better Health System,9Computational Technology for Effective Health Care,10Digital Infrastructure for the Learning Health System,11 and Best Care at Lower Cost: The Path to Continuously Learning Health Care in America.12 These reports build upon an exceptional foundation of Institute of Medicine (IOM) reports issued in the late 1990s and the 2000s. They share a common goal – utilizing technology and informatics to define a research agenda/strategy for studying the issues and challenges surrounding the transformation of the practice and delivery of healthcare.
The National Institutes of Health National Center for Advancing Translational Sciences led Clinical Translational Science Awards, the Big Data to Knowledge initiative,13 and the Patient-Centered Outcomes Research Institute programs are changing the landscape of health research. With the rapid implementation of electronic health records (EHRs) and the integration of EHR data into clinical data repositories (CDRs), large quantities of clinical data are now available. These data can, together with state-of-the-art computational technologies, stimulate translational science. However, nursing data, which represents the largest portion of EHR documentation, is seldom included in such CDRs and is not often used for translational research.
Historical context
Over the past 40 years, the nursing discipline has identified, defined, and coded essential clinical and contextual data, but these data have not been consistently or widely integrated into EHRs, administrative systems, or CDRs to support translational research. Beginning in 1989, the American Nurses Association (ANA) developed a process for recognizing terminologies that represent nursing knowledge; the process was later updated to be consistent with International Organization for Standardization requirements.14 The Nursing Minimum Data Set and the Nursing Management Minimum Data Set (NMMDS) provide umbrella concepts representing the practice and context of nursing care.15,16 Discrete terminologies recognized by the ANA cover assessments, problems (diagnoses), interventions, and outcomes that address human responses to health and wellness.17,18 The first nursing terminology, the North American Nursing Diagnoses Association, was developed in 1973, followed by the Omaha System, Nursing Interventions Classification, Perioperative Nursing Data Set, Clinical Care Classification, International Classification of Nursing Practice, and Nursing Outcomes Classification.14 These data sets and terminologies were recognized by the ANA, in addition to two interprofessional terminologies: Logical Observation Identifiers Names and Codes (LOINC), to represent laboratory and clinical observations (assessments), and the Systematized Nomenclature of Medicine Clinical Terms (SNOMED CT), which includes findings, problems, interventions, and outcomes.
Beginning in 1994, the ANA launched two efforts to create sharable and comparable nursing data for secondary use. In that year, the ANA created a national CDR to support patient safety and quality improvement through comparison of hospital data – the National Database for Nursing Quality Indicators (NDNQIs).19 This was an important first step in demonstrating the value of nursing data in CDRs, but representation of nursing quality in this database continues to be limited, due to the voluntary nature of submissions, the small number of participating hospitals, and the fact that data are often collected manually. Furthermore, standard nursing terminologies are not part of the database’s requirements, since many hospitals are still transitioning from paper to digital documentation and, therefore, have not yet considered using standardized terminologies. As early as 1997, the ANA developed criteria to evaluate and recognize vendors whose information systems meet the requirements for linking nursing terminologies to quality outcomes.20 The Certification Commission for Healthcare Information Technology has similar criteria for EHR certification. Although the Office of the National Coordinator (ONC) later adopted these criteria, the ONC’s version of the criteria no longer included nursing data.
There are additional efforts to integrate nursing data into EHRs and use these data for business operations and research, but nursing terminologies have not been widely adopted. Terminology developers and individual EHR vendors have been working separately to determine which terminology to use, the best way to integrate the terminologies into their EHRs, and how to demonstrate the value of successfully integrating nursing terminologies in practice. A collaborative effort between healthcare organizations and vendors could greatly enhance and expedite the adoption of standardized nursing terminologies for secondary use and translational science.
Challenges to achieving sharable and comparable nursing data
There are several challenges that further impede the implementation of nursing terminologies and information structures within EHRs, and their subsequent use for research (see Figure 1). These challenges can be categorized into four dimensions: knowledge, practice, policies/resources, and research.
Figure 1:
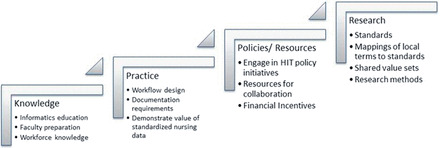
Challenges to Achieving Sharable and Comparable Nursing Data
First, the knowledge needed to develop and champion sharable and comparable nursing data is unevenly distributed in nursing education programs. Nursing programs are required to teach technology and informatics at all education levels (except PhD); however, they are not required to include nursing terminologies in their curriculums.21 Additionally, nursing faculties are ill prepared to teach these subjects, due to a lack of knowledge regarding nursing terminologies, their use in EHRs, and their potential for transforming healthcare. As a result, the nursing workforce is still not prepared to request, require, use, or value the use of standardized nursing data. Nursing was one of the first disciplines to have informatics certification; however, that certification includes a minimum of a baccalaureate degree and does not address advanced informatics practice. Increasing education in this domain will be difficult without acknowledging advanced practice knowledge, including standard terminology use and application, in informatics.
The second challenge is practice. Evidence is emerging for the value of nursing data and the potential of standardized nursing documentation models/frameworks and data standards to, primarily, support efficient, complete, and accurate information in practice and, secondarily, to support quality improvement, business analytics, and research. Nurse satisfaction with EHR workflow design’s ability to streamline documentation22 has been the focus of most research, rather than how EHR design affects the safety, quality, and costs of care. Nursing documentation provides data for reporting quality metrics, such as prevention of pressure ulcer or falls. EHRs could reduce the costs of reporting quality measures, but that would require implementing consistent documentation models, data standards, and the ability to export data for reports, rather than hiring data abstractors/chart reviewers. Resistance to change may also present a barrier within practice, as providers are unaccustomed to relying on protocols founded on evidence-based practice guidelines and translational research that uses big data analytic strategies.23 The lack of nursing executive and clinician workforce knowledge regarding standardized processes and data is limited, even in standard development organizations such as HL7. The links between structured data, analytic strategies for that data, and the benefits the data may generate are not widely understood. Therefore, demand for and resourcing of implementation and secondary use of clinical nursing data, enabled by nursing terminologies and information structures embedded in EHRs, is limited or not supported.
The third challenge regards national health policy and resources for implementation and subsequent use of standardized nursing terminologies and information structures for business analytics and research. Incentive payments for meeting meaningful use of EHR standards do not include nursing-derived data, with the exception of specific instances of data documented by advanced practice nurses caring for Medicaid patients. Moreover, health policies and regulations such as Accountable Care Organizations and the requirements for implementation of ICD-10 do not include provisions for integrating nursing terminologies (including SNOMED CT and LOINC, which are required) into EHRs. Because meaningful use of EHRs requires common data standards, the multiplicity of nursing terminologies presents a challenge for health systems integration, health information exchange, and comparative effectiveness across systems. However, there are solutions. The ONC recommends LOINC and SNOMED CT for eMeasures. ANA recognizes both these terminologies as representing nursing knowledge. To use LOINC for assessments and SNOMED CT for findings, nursing problems, interventions and outcomes when exchanging data and building CDRs, consensus much be reached. This does not preclude the use of any ANA-recognized terminology; rather LOINC and SNOMED CT provide an essential common data standard for comparative effectiveness and big data research across systems. The National Library of Medicine (NLM) supplies terminology mappings, but only some ANA-recognized terminologies are current and, therefore, mapped to LOINC or SNOMED CT. In addition, some mappings are not available in the NLM’s Unified Medical Language System. Furthermore, tutorials and open-source, collaborative tools are needed to demonstrate how nursing data can be mapped to the common standards recommended by the ONC.
The last challenge (depicted in Figure 1) is research. There is a considerable body of research on the impact of nursing on health and healthcare, including the 10 landmark nursing research studies published by the National Institute of Nursing Research (NINR) and the 2010 IOM Future of Nursing report.24,25 However, enabling such research at a coordinated, efficient, and national level with the secondary use of EHR data is in an infant stage. Informatics and newer methods of secondary use of data in doctoral programs must be addressed. The NINR supports Big Data Science26; however, nurse researchers may not be prepared to participate in or compete for grants using big data. In a recent evaluation of the content from 120 US nursing PhD programs’ websites, only 22.5% mentioned course work or research experiences in informatics.27 To properly educate future researchers, advanced nursing degrees need to impart knowledge and skills for developing science, stewarding the discipline, and addressing the new methodologies emerging in big data and science to doctoral students.
Although many disparate individuals and organizations are addressing the need for standardized nursing data integration into EHRs, its subsequent use for research, and its potential to transform health care, there is limited coordination of their efforts. National consensus and a national action plan are needed to coordinate integration activities and overcome challenges to implement and use sharable and comparable nursing data in EHRs and CDRs to support research. While new work may be needed, a national action plan would primarily emphasize identifying and harmonizing exemplary existing work and would only initiate new work when needed.
CONSENSUS CONFERENCE
In August 2013, the University of Minnesota School of Nursing and its Center for Nursing Informatics hosted a group of 40 leaders/organization stakeholders at the inaugural Nursing Knowledge: Big Data Research to Transform Health Care consensus conference. Participants were invited based on their expertise and to represent a diverse range of organizations: practice settings (health systems, community-based settings), education (both university educators and nurses from the American Association of Colleges of Nursing and the National League for Nursing), informatics organizations (American Medical Informatics Association (AMIA), Health Information Management Systems Society (HIMSS) Alliance for Nursing Informatics, American Academy of Nursing Informatics Expert Panel), research (NINR), standards organizations (LOINC, HL7, IHE, and the ONC Standards and Interoperability Framework), federal and state organizations (National Quality Forum, Minnesota e-Health Initiative), national nursing specialty organizations, EHR and other informatics vendors, and potential funding organizations (NINR, Agency for Healthcare Research and Quality, Robert Wood Johnson Foundation).
The purpose of this invitational conference was to create a national action plan to harmonize existing individual and organizational efforts to ensure that the knowledge and information that nurses generate are consistently integrated into CDRs. Ultimately, the data can be utilized as a source of insights and evidence to transform healthcare and improve outcomes for patients. Prior to the conference, white papers with a myriad of resources were provided as background, emphasizing the national vision, federal initiatives, and nursing efforts, as well as the proposed value of sharable and comparable nursing data.28 Gathered in Minneapolis for a 2-day conference, participants created a collaborative course of action to:
Integrate nursing information into EHRs.
Implement standardized language to represent nursing assessments, diagnoses, interventions and outcomes of care.
Modify and standardize nursing informatics education to build knowledge and competency.
Influence policy and standards for documenting and coding nursing information in healthcare knowledge systems.
Proceedings from the conference, “2013 Nursing Knowledge: Big Data Research for Transforming Healthcare,” are available online.28,29 The 2013 Action Plan primarily focused on harmonizing ongoing activities and filling in gaps with new activities where needed.
Building on the 2013 conference and earlier informatics work, in June 2014, the second Nursing Knowledge: Big Data and Science for Transforming Health Care conference brought together more than 70 stakeholders from nursing practice, education, information technology, professional nursing, and informatics and standards organizations. It included the 2013 invitees and additional participants, through open registration. This 2014 consensus conference included report-outs on activities and accomplishments related to the 2013 Nursing Knowledge conference action plan and associated recommendations for further developing the national action plan for building sharable and comparable nursing data. Accomplishments were either new activities or existing work that was now aligned with a common vision for sharable and comparable nursing data to expand large clinical data sets for research. The steering committee synthesized preliminary recommendations from abstracts submitted by presenters prior to the conference. Following each group of presentations, participants joined small work groups to refine preliminary action items and brainstorm new strategies and action steps for 2014. Each group then presented their recommended “actions” to the entire assembly. The conference concluded with an “action auction.” Attendees bid on (volunteered) to participate in actions that they as individuals or their organizations were willing to advance in the next year, (1) to ensure that sharable and comparable nursing information would be included in EHRs and (2) to ensure that all domains of the nursing profession are knowledgeable about the potential of very large clinical data sets (or big data) to transform practice, research, and education.
2014 NATIONAL ACTION PLAN
The complete proceedings of the 2014 conference are publicly available and include a summary of the conference, attendees, abstracts and slides from the presentations, accomplishments related to the 2013 National Action Plan for Big Data and Nursing, and the new 2014 National Action Plan.30 Ten action teams were formed as a result of the conference, as shown in Table 1. The action teams have long-term objectives, and also focus some near-term deliverables. Participants committed to reporting their teams’ achievements and challenges by June 4, 2015 at the next Nursing Knowledge: Big Data Research to Transform Health Care conference. Putting new and existing ideas into practice, as exemplified by the action teams, is key to the success of the conference. In the past, many of the same people and organizations worked to achieve the goal of sharable and comparable nursing data to support practice and translational science. However, they worked in isolation. Never before has the breadth of participation, nor the high level of expertise, been brought together. In fact, all constituencies that influence policy and practice are included in the teams: practice, research, education, federal regulators, vendors, and professional organizations. This strategy is structured to achieve what no organization, such as ONC, could do alone. (The full membership and organizational representation of each of the teams can be found on the conference’s website.)
Table 1:
2014 National Action Plan Teams/Coordinators
| Challenges | Action team description/team coordinators |
|---|---|
| Education |
|
| |
| Practice |
|
| |
| Policies/incentives |
|
| |
| |
| Research |
|
| |
|
Individual teams meet virtually to prioritize the most impactful actions (that can be completed in <12 months) to overcome challenges within education, practice, national policies and incentives, and research. Team leaders meet monthly to ensure coordination of actions, deliverables, and problem-solving. To guarantee that actions reach fruition, teams implement consistent follow up and use of shared resources. Web-based project management software (Basecamp) allows teams to schedule meetings, track progress on actions, email reminders for task due dates, collaborate on work, share documents, and provide transparency of all of the work within and across teams.
Education
Two of the action teams identified in Table 1 address education. While inclusion of informatics in most levels of nursing education is required, there is no consensus about standardizing curriculum content. One of the action teams is developing national consensus on a standard curriculum for prelicensure nursing students. Creating a national advisory board of key leaders in nursing informatics will support building consensus and identifying informatics competencies, including capturing and using nursing data as well as ensuring the quality of data from patients throughout the care process. Subsequently, resources for curriculum improvement will be developed through a robust education metadata repository of tools to share standards and recommendations for evidence-based practice. Building on AMIA’s work to board certify physicians in clinical informatics, the second team collaborates with AMIA and the Commission on Accreditation for Health Informatics and Information Management Education to create advanced informatics certification and accreditation for nurses and other health professionals. Team members are gathering information about individual certification, individual credentialing, and program accreditation in informatics programs. Their efforts will foster interprofessional education and preparation for advanced informatics certification and accreditation.
Practice
Two teams are addressing the optimization of EHR documentation and demonstrating the value of nursing data. One of their major focuses is to identify opportunities to support nursing within EHRs and capture nursing’s contribution to quality, safety, reliable care, and patient engagement. This team will identify the information structures and infrastructures needed within EHRs and CDRs to enable the storage, aggregation, and querying of nursing data at an organizational level. The structures will also support data exchange at the national or international levels, to support quality outcomes, practice-based evidence, and knowledge representation. The teams will share their work through collaboration with diverse leaders from practice, researchers, and vendors via a set of recommendations for integrating the best clinical knowledge into care decisions.
Demonstrating the value of integrating standardized nursing data into EHRs is the focus of the second practice team. The team is developing a national consensus model to measure patient-level nursing intensity and costs as well as to produce metrics, to benchmark nursing care finance, combined with clinical care, to estimate nursing value. They are also identifying new business intelligence and analytic tools that 1) utilize the clinical, operational, financial, and outcomes data currently available in the EHR, and 2) foster integration into different health care settings. These new business intelligence and analytic tools will enable the creation of “accountability dashboards” for nurses, which can be used for learning, evidence building, and understanding the impact of nursing.
Policies/resources
Health IT policies shape the requirements, resources, and financial incentives for creating standardized data that can be used to create large clinical data sets and conduct research. However, nurses are underrepresented on national and international working groups/committees such as the ONC, standards organizations, or the National Quality Forum. Implementation strategies that advance the adoption of standardized terminologies and information structures for clinical documentation by nurses in EHRs need policy and resource support. Consequently, an additional team is focusing on engaging nurses in health IT committees and workgroups, which includes providing stakeholders with background information about advocating for the inclusion of standardized nursing data and frameworks. This group will foster nurses’ engagement in policy dialogues, including webinars, to drive national policies, and nursing and health stakeholder consensus, in support of harmonizing nursing content into national and international standards.
A major health IT policy effort is the creation of eMeasures, for demonstrating meaningful use of EHR data. Efforts are underway through the National Database of Nursing Quality Indicators to create an eMeasure for pressure ulcers and to recommend its inclusion in Stage 3 of EHR Meaningful Use. This effort includes not only the reliability, validity, and feasibility testing of the eMeasure, but also political action to assure inclusion in Meaningful Use Stage 3. The team will collaborate with the ANA to both ensure the adoption of the Pressure Ulcer eMeasure for meaningful use and to encourage vendors and EHR users to implement the eMeasure.
Standardized nursing data includes administrative or workforce data as well as EHR data. The IOM’s 2010 Future of Nursing25 report recommends that 80% of nurses be prepared for entry into practice at the baccalaureate level, and also states that the number of faculty who are prepared at the doctoral level must increase to achieve this goal. Consistent collection of workforce data is needed. The data elements of the ANA-recognized NMMDS terminology have been normalized to national definitions, coded in LOINC, and made publicly available for dissemination through LOINC. An implementation guide and communication plan will be developed within the year. Moreover, the team will work with the Robert Wood Foundation Initiative on the Future of Nursing and the State Boards of Nursing to collect comparable workforce data. A further initiative includes collaborating with the ONC Health IT Policy Committee, Certification and Adoption Workgroup, and Workforce Subgroup to ensure that nursing is identified in the ongoing efforts to develop a Standard Occupational Code for Health Informatics Practitioners.
Research
Foundational and applied research methods to conduct research with big data (that includes nursing data) are essential. The ONC recommends the use of LOINC for coding assessments and SNOMED CT for problems, procedures (interventions), and outcomes. The ANA recognizes both these terminologies, and both can be used for normalizing data, including nursing data, for health information exchange and creation of CDRs to support comparative effectiveness and translational research. However, further work is needed to determine the coverage of these terminologies for nursing data, integrate new codes where needed, and disseminate LOINC and SNOMED CT using a framework for integration into EHRs. To advance this goal, one team is addressing the completeness of LOINC for representing nursing assessments and harmonizing SNOMED CT for consistent use.
A second team is focusing on the harmonization and standardization of nursing data and related models. This group’s work seeks to move beyond assuring standardization of terminology into the realm of nursing knowledge by addressing the integration of nursing terminologies across the continuum of care and maintaining actionable and relevant documentation of the patient’s care plan. The team is developing and testing models that can make data actionable and respond to continual regulatory changes that are dependent on national and global economic conditions. They will also create a common repository for sharing data models and coding nursing data to prevent duplication of effort across researchers, health systems, and EHR vendors.
Moving beyond the foundational work, nurses must commit to using standardized nursing data from EHRs. One team is focused on engaging nurse researchers, particularly those involved with Clinical Translational Science Awards or Patient-Centered Outcomes Research Institute grants, to advocate for the inclusion of nursing data in CDRs and for its use in research. A review of the literature, aimed at identifying current applied informatics research methods and recommending the need for newer, more practical big data science methods, is in progress. A recent data mining study demonstrates one of the newer applied research methods by exploring the influence of nursing interventions on outcomes, such as those for the frail elderly and preventing rehospitalization.31 The team will support ongoing efforts both for research and business analytics to use nursing data for predictive modeling. Finally, the team will demonstrate these methods at the 2015 Nursing Knowledge Big Data and Science conference.
Researchers conducting symptom science work have acknowledged the need for coded data in CDRs. They recognize that it is essential to have coded data recorded by nurses that describe patient symptoms, use common data elements, and store the data in designated data repositories. In an article, “Envisioning the Future in Symptom, Science,” the consortium states “as the complexity of symptom etiology and expression becomes, clear, new approaches and technologies are needed to better address biology and context, common data sources need to be built and shared, and addressing the impact of empirical findings on health policy.”32(p346) This recognition of the need for standardized data and information structures (the domain of nursing informatics) is an indication that researchers finally understand the need for this type of patient data, instead of creating new concepts and terms around their own theoretical frameworks without regard for their clinical use.
CONCLUSION
The 2014 National Action Plan for Sharable and Comparable Nursing Data for Transforming Health and Healthcare builds on and seeks to coordinate existing, but separate, long-standing efforts of many individuals and organizations. The plan is action-focused, with designated accountability for coordinating and tracking progress. Foundational to integrating nursing data into CDRs for big data science and research is the implementation of standardized nursing terminologies, common data models, and information structures within EHRs. The 2014 plan builds on existing federal health policies for standardized data that are relevant to meaningful use of EHRs and clinical quality eMeasures. It also establishes directions to expand health policies to incorporate sharable and comparable nursing data, as well as to expand the means of using that data for research. Next steps will include a follow-up conference in June 2015 to report accomplishments, continue to foster collaboration between initiatives and organizations, and support consensus on the standardization of nursing data in practice, education, and research.
CONTRIBUTORS
All authors had a substantial contributions to the 1) conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; 2) drafting the work or revising it critically for important intellectual content; 3) final approval of the version to be published; and 4) agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
COMPETING INTEREST
None.
Supplementary Material
REFERENCES
- 1. Institute of Medicine (IOM). To Err is Human: Building a Safer Health System .Committee on Quality of Health Care, ed. Washington, DC: National Academies Press; 1999. [Google Scholar]
- 2. Institute of Medicine (IOM). Crossing the Quality Chasm: A New Health System for the 21st Century .Committee on Quality of Health Care in America, ed. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 3. Institute of Medicine (IOM). Improving the Quality of Long-term Care .Committee on Improving Quality in Long-Term Care, ed. Washington, DC: National Academies Press; 2001. [Google Scholar]
- 4. Institute of Medicine (IOM). Keeping Patients Safe: Transforming the Work Environment of Nurses .Committee on the Work Environment for Nurses and Patient Safety, ed. Washington, DC: National Academies Press; 2004. [Google Scholar]
- 5. Institute of Medicine (IOM). Health Professions Education: A Bridge to Quality .Committee on the Health Professions Education Summit, 1st ed. Washington, DC: National Academies Press; 2003. [Google Scholar]
- 6. Institute of Medicine (IOM). Insuring America's Health: Principles and Recommendations .Committee on the Consequences of Uninsurance, ed. Washington, DC: National Academies Press; 2004. [Google Scholar]
- 7. Van Den Bos J, Rustagi K, Gray T, et al. The $17.1 billion problem: The annual cost of measurable medical errors. Health Aff. 2011;30(4):596–603. [Google Scholar]
- 8. Landrigan C, Landrigan G, Parry C, et al. Temporal trends in rates of patient harm resulting from medical care. N Engl J Med. 2010;363(22):2124–2134. [DOI] [PubMed] [Google Scholar]
- 9. Institute of Medicine (IOM). Health IT and Patient Safety: Building Safer Systems for Better Care .Committee on Patient Safety and Health Information Technology, ed. Washington, DC: National Academies Press; 2011. [Google Scholar]
- 10. National Research Council. Computational Technology for Effective Health Care: Immediate Steps and Strategic Directions .Washington, DC: National Academies Press; 2009. [Google Scholar]
- 11. Institute of Medicine (IOM). Digital infrastructure for the Learning Health System: The Foundation for Continuous improvement in health and Health Care: Workshop Series Summary .Washington, DC: National Academies Press; 2011. [Google Scholar]
- 12. Institute of Medicine (IOM). Best Care at Lower Cost: The Path to Continuously Learning Health Care in America .Washington, DC: National Academies Press; 2012. [Google Scholar]
- 13. National Institutes of Health. Big data to knowledge (BD2K) initiative. http://bd2k.nih.gov/#sthash.F4fUFExw.dpbs. Accessed July 7, 2014. [Google Scholar]
- 14. Westra BL, Delaney CW, Konicek D, Keenan G. Nursing standards to support the electronic health record. Nurs Outlook. 2008;56(5):258–266. [DOI] [PubMed] [Google Scholar]
- 15. Werley HH, Lang NM, eds. Identification of the Nursing Minimum Data set .New York, NY: Springer Publishing Company; 1988. [Google Scholar]
- 16. Huber D, Schumacher L, Delaney C. Nursing management minimum data set (NMMDS). J Nurs Adm. 1997;27(4):42–48. [Google Scholar]
- 17. American Nurses Association. ANA recognized terminologies and data element sets. http://nursingworld.org/npii/terminologies.htm. 2007. Accessed July 5, 2007. [Google Scholar]
- 18. Lundberg C, Brokel JM, Bulechek GM, et al. Selecting a standardized terminology for the electronic health record that reveals the impact of nursing on patient care. J Nurs Inform. 2008;12(2):19p. [Google Scholar]
- 19. Montalvo I. The National Database of Nursing Quality Indicators (NDNQI). Online J Issues Nurs. 2007;12(3):13p. [PubMed] [Google Scholar]
- 20. American Nurses Association (ANA). NIDSEC: Standards and scoring guidelines. (reproduced with permission of the American nurses association). http://z.umn.edu/nidsec. Accessed January 2, 2015. [Google Scholar]
- 21. American Association of Colleges of Nursing (AACN). Essentials Series. http://www.aacn.nche.edu/education-resources/essential-series. Updated 2013. Accessed January 11, 2013. [Google Scholar]
- 22. Carayon P, Cartmill R, Blosky MA, et al. ICU nurses’ acceptance of electronic health records. J Am Med Inform Assoc. 2011;18(6):812–819. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Groves P, Kayyali B, Knott D, Van Kuiken S. The Big-data Revolution in Healthcare: Accelerating Value and Innovation. Center for US health system reform: Business technology office, McKinsey&Company. http://www.mckinsey.com/insights/health_systems_and_services/the_big-data_revolution_in_us_health_care. Updated 2013. Accessed September 8, 2014. [Google Scholar]
- 24. National Institute of Nursing Research. Changing Practice, Changing Lives: 10 Landmark Nursing Research Studies. https://www-ninr-nih-gov.ezp2.lib.umn.edu/newsandinformation/publications#.VAHZfmPQpWs. Updated n.d. Accessed August 29, 2014. [Google Scholar]
- 25. Institute of Medicine (IOM). The Future of Nursing: Leading Change, Advancing Health .Washington, DC: The National Academies Press; 2010. [Google Scholar]
- 26. National Institute for Nursing Research (NINR). NINR big data methodologies boot camp. https://www.ninr.nih.gov/training/trainingopportunitiesintramural/bootcamp#.VA8QDmPQpWs. Updated 2014. Accessed September 9, 2014. [Google Scholar]
- 27. Wyman JF, Henly SJ. PhD programs in nursing in the United States: visibility of AACN core curricular elements and emerging areas of science. Manuscript submitted for publication. 2014. [Google Scholar]
- 28. Westra BL, Delaney CW, Matney S, et al. 2013 Nursing Knowledge Big Data Research for Transforming Healthcare: Pre-conference Resources .http://www.nursing.umn.edu/about/calendar-of-events/2013-events/big-data-2013/Pre-ConferenceMaterials/index.htm. Updated 2013. Accessed August 30, 2014. [Google Scholar]
- 29. Clancy TR, Bowles KH, Gelinas L, et al. A call to action: Engage in big data science. Nurs Outlook. 2014;62(1):64–65. [Google Scholar]
- 30. Delaney CW, Westra BL, Latimer GE, et al. 2014 Nursing Knowledge: Big Data & Science for Transforming Health Care Conference. http://www.nursing.umn.edu/about/calendar-of-events/2014-events/big-data-2014/index.htm. Updated 2014. Accessed August 30, 2014. [Google Scholar]
- 31. Monsen KA, Westra BL, Oancea SC, Yu F, Kerr MJ. Linking home care interventions and hospitalization outcomes for frail and non-frail elderly patients. Res Nurs Health. 2011;34:160–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Corwin EJ, Berg JA, Armstrong TS, et al. Envisioning the future in symptom science. Nurs Outlook. 2014;62(5):346–351. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


